Gary Taubes paints a lively picture of lawmaker overzealousness, industry subterfuge, and researcher bias to argue that fat may have been unfairly blamed for the ravages of sugar, and as a result, misguided government dietary advice drove Americans to eat more sugar, ultimately contributing to obesity, diabetes, and coronary heart disease. Yet the key questions Taubes raises cannot be evaluated via historical narrative. It’s time to hang up our tweed blazers and slip into our white lab coats, because Taubes has made specific and testable assertions, which I will evaluate in three parts. First, I will examine the 1980 Dietary Guidelines to determine if they condemn fat and take a weak stance on sugar as suggested. Second, I will evaluate the hypothesis that the Guidelines contributed to obesity, diabetes, and coronary heart disease. And third, I will evaluate the hypothesis that sugar “may be the primary cause” of the three aforementioned conditions.
Inside the 1980 Dietary Guidelines for Americans
In the opening sentence of his essay, Taubes states that “forty years ago this month, January 1977, the federal government entered the business of giving dietary advice,” referring to a congressional report that gave rise to the 1980 Dietary Guidelines for Americans. In fact, the federal government has been issuing dietary advice regularly for over a century.[1] The 1980 Guidelines were, however, notable for the fact that they abandoned the traditional “eat more” approach of diversifying and balancing the diet, in favor of an “eat less” approach of limiting foods perceived as unhealthy.[2]
Taubes argues that this document condemned fat and took a weak stance on sugar. Let’s have a look for ourselves.[3] At the core of the 1980 Guidelines were seven pieces of dietary advice, shown below:
As you can see, “avoid too much fat” and “avoid too much sugar” are equally prominent and identically worded recommendations. Taubes suggests that the statement “avoid too much sugar” is vague and lacks conviction—it is “a tautological statement that could apply to any food.” Yet we are intended to believe that the same language applied to fat altered the course of the American diet.
The Guidelines went further, providing explicit guidance on how to “avoid too much sugar”:
- Use less of all sugars, including white sugar, brown sugar, raw sugar, honey, and syrups.
- Eat less of foods containing these sugars, such as candy, soft drinks, ice cream, cakes, cookies.
In the section titled “Maintain Ideal Weight,” the document lays out its four-part plan for weight loss: Increase physical activity, eat less fat and fatty foods, eat less sugar and sweets, and avoid too much alcohol. Again, the advice to limit fat and sugar intake receive equal attention, and the Guidelines clearly implicate excess sugar intake in obesity.
A person who faithfully adhered to the Guidelines would end up eating a diverse, largely unprocessed diet composed of whole grains, beans, nuts, lean meats, seafood, dairy, eggs, vegetables, and fruits, with little added sugar, added fat, or highly processed foods or beverages. Are we really to believe that this advice—which clearly and repeatedly recommended eating less sugar—made Americans eat more sugar, leading to obesity, diabetes, and coronary heart disease? Having reviewed the Guidelines, the notion strains credulity, but let’s test it anyway.
Wrath of the Guidelines
Taubes argues that the Guidelines may have unintentionally contributed to obesity, diabetes, and coronary heart disease. This rests on the assumption that the Guidelines themselves substantially influenced American eating behavior, either directly or indirectly via the food industry, and therefore that changes in the American diet over time can be attributed to it rather than to the numerous other shifts in the American food and cultural landscape that were happening at the time.[4] No evidence is presented to support this assumption, so we will examine it here.
If the Guidelines substantially influenced the American diet, then we should observe that total fat, added fat, and added sugar intake declined in its wake. In perfect contrast to this prediction, our total intake of fat remained approximately the same after the Guidelines, our intake of added fat increased, and our intake of added sugar increased.[5],[6]
Furthermore, we should observe a decline in the consumption of highly processed foods rich in fat and sugar that the Guidelines clearly advised against. To test this prediction, here are the top six sources of calories in the U.S. diet, in descending order of importance, as of 2006:
- Grain-based desserts (cakes, cookies, donuts, pies, and related items)
- Yeast breads
- Chicken and chicken-mixed dishes
- Soda, energy drinks, and sports drinks
- Pizza
- Alcoholic beverages[7]
This list is both disturbing and informative. Cake and related desserts are the number one source of calories in the American diet. Soda, pizza, and alcohol are three of the remaining five items. The average American diet is not even remotely inspired by the Guidelines.
The truth is that we don’t wash down our pizza and cake with beer and soda because we think it’s healthy or because we believe the government recommended it. We do it because we are human beings who are driven by considerations of pleasure, cost, and convenience—precisely the qualities the food industry has been optimizing for the last 40 years.[8]
Taubes assumes that we suffer from increasing rates of obesity and diabetes because we have failed to identify their true cause. Yet the evidence suggests a simpler and more compelling explanation: We eat too much food that is obviously unhealthy, and it’s not because researchers or the government told us to, but because we like it.
A Slow-Acting Toxin
According to Taubes, sugar may be a “toxin” and “the primary cause of diabetes, independent of its calories, and perhaps of obesity as well.” Elsewhere in the essay, coronary heart disease is added to the list. Yet Taubes asserts that this speculative hypothesis cannot currently be tested because there is so little existing research on sugar, and so little interest in conducting such research, that “the research necessary to nail it down would take years to decades to complete and is not even on the radar screen of the funding agencies.”
This belief is remarkable in light of the fact that a Google Scholar search returns hundreds of scientific papers on the health impacts of sugar, many of them human randomized controlled trials, and many funded by the U.S. National Institutes of Health. In reality, the health impacts of sugar are of considerable interest to the scientific community, and as such, they have been studied extensively. Having established that this research exists, let’s take a look at it.
The hypothesis that sugar is the primary cause of coronary heart disease is easily refuted. In the United States, coronary heart disease mortality has plummeted by more than 60 percent over the last half century, despite a 16 percent increase in added sugar intake.[9] Roughly half of this decline can be attributed to better medical care, while the other half is attributed to underlying drivers of disease such as lower cholesterol and blood pressure levels and an impressive drop in cigarette use.[10]This striking inverse relationship is incompatible with the hypothesis that sugar is the primary cause of coronary heart disease, although it doesn’t exonerate sugar.
Is sugar the primary cause of diabetes, “independent of its calories”? Research suggests that a high intake of refined sugar may increase diabetes risk, in large part via its ability to increase calorie intake and body fatness, but it is unlikely to be the primary cause.[11] An immense amount of research, including several large multi-year randomized controlled trials, demonstrates beyond reasonable doubt that the primary causes of common (type 2) diabetes are excess body fat, insufficient physical activity, and genetic susceptibility factors.[12]
The ultimate test of the hypothesis that sugar is the primary cause of obesity and diabetes would be to recruit a large number of people—perhaps even an entire country—and cut their sugar intake for a long time, ideally more than a decade. If the hypothesis is correct, rates of obesity and diabetes should start to decline, or at the very least stop increasing. Yet this experiment is far too ambitious to conduct.
Or is it? In fact, this experiment has already been conducted—in our very own country. Between 1999 and 2013, intake of added sugar declined by 18 percent, taking us back to our 1987 level of intake. Total carbohydrate intake declined as well.[13] Over that same period of time, the prevalence of adult obesity surged from 31 percent to 38 percent, and the prevalence of diabetes also increased.[14]
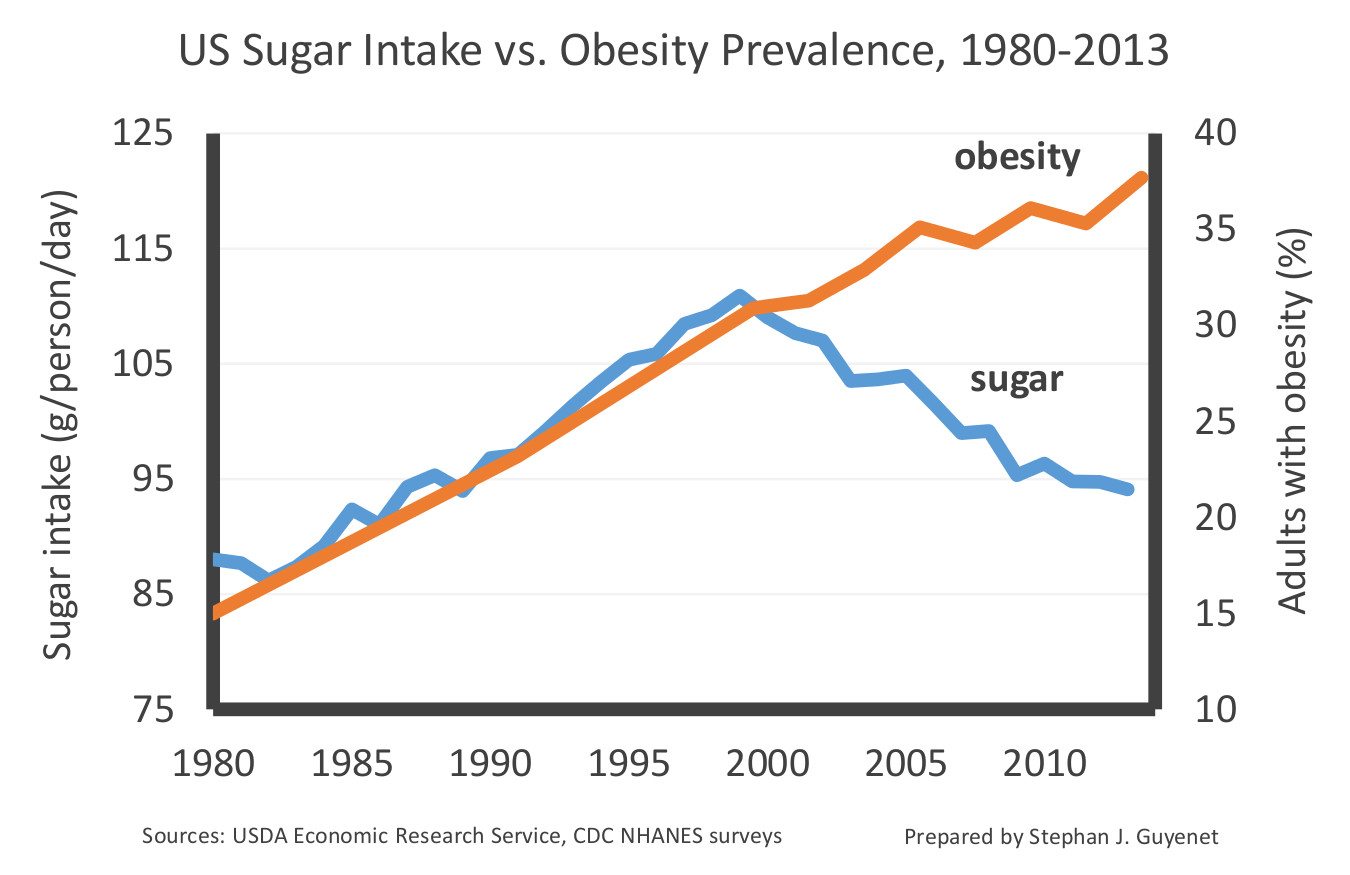
U.S. sugar intake and adult obesity prevalence, 1980-2013. Data are from Centers for Disease Control and Prevention NHANES surveys and USDA Economic Research Service food disappearance records (5,6). Axes are bounded to illustrate correlation, or lack thereof.
Americans have been reining in our sugar intake for more than fourteen years, and not only has it failed to slim us down, it hasn’t even stopped us from gaining additional weight. This suggests that sugar is highly unlikely to be the primary cause of obesity or diabetes in the United States, although again it doesn’t exonerate sugar. Furthermore, it suggests that the laser-like focus on sugar is a distraction from the true, more complex nature of the problem.
I have presented a small piece of a large body of evidence that is more than sufficient to refute the assertion that sugar may be the primary cause of obesity, diabetes, and coronary heart disease. At the same time, this evidence does suggest that added sugar is part of a broader diet and lifestyle landscape that contributes to these three conditions, a conclusion that is not especially controversial within today’s scientific, medical, and public health communities.
[1] Davis C, Saltos E. Dietary Recommendations and How They Have Changed Over Time. USDA Economic Research Service; 1999.
[2] Nestle M. Food Politics: How the Food Industry Influences Nutrition, and Health, Revised and Expanded Edition. Berkeley: University of California Press; 2007. 510 p.
[3] Nutrition and Your Health. Dietary Guidelines for Americans. US Department of Agriculture and US Department of Health and Human Services; 1980.
[4] For example, the declining cost of sweeteners and processed food in general, increasing ubiquity of food and advertising, advances in food sensory engineering, and the replacement of home cooking with restaurant and pre-prepared food. I discuss these trends in my book The Hungry Brain.
[5] Taubes has previously argued that the percentage of fat in the U.S. diet declined in the wake of the Guidelines, which is correct. However, this percentage change was due to an absolute increase of carbohydrate intake, not an absolute decline of fat intake. Since our absolute intake of fat remained unchanged, this cannot be interpreted as a decline of fat intake. USDA Economic Research Service - Food Availability (Per Capita) Data System [Internet]. 2016 [cited 2016 Dec 22]. Available from: https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/. Austin GL, Ogden LG, Hill JO. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971-2006. Am J Clin Nutr. 2011 Apr;93(4):836–43.
[6] Throughout this piece, the term “added sugar” refers to table sugar, high-fructose corn syrup, honey, and all other calorie-containing sweeteners, including both home use and consumption via prepared foods and beverages. It does not include the sugar naturally found in fruit, vegetables, and milk.
[7] U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. U.S. Government Printing Office; 2010.
[8] Moss M. Salt Sugar Fat: how the food giants hooked us. New York: Random House; 2013.
[9] Ibid. See also USDA, above, and Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004 Aug 3;110(5):522–7. And Ford ES, Roger VL, Dunlay SM, Go AS, Rosamond WD. Challenges of ascertaining national trends in the incidence of coronary heart disease in the United States. J Am Heart Assoc. 2014 Dec 3;3(6):e001097.
[10] Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007 Jun 7;356(23):2388–98.
[11] Horst KW ter, Schene MR, Holman R, Romijn JA, Serlie MJ. Effect of fructose consumption on insulin sensitivity in nondiabetic subjects: a systematic review and meta-analysis of diet-intervention trials. Am J Clin Nutr. 2016 Dec 1;104(6):1562–76. Black RNA, Spence M, McMahon RO, Cuskelly GJ, Ennis CN, McCance DR, et al. Effect of eucaloric high- and low-sucrose diets with identical macronutrient profile on insulin resistance and vascular risk: a randomized controlled trial. Diabetes. 2006 Dec;55(12):3566–72. Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009 May;119(5):1322–34. Lewis AS, McCourt HJ, Ennis CN, Bell PM, Courtney CH, McKinley MC, et al. Comparison of 5% versus 15% sucrose intakes as part of a eucaloric diet in overweight and obese subjects: effects on insulin sensitivity, glucose metabolism, vascular compliance, body composition and lipid profile. A randomised controlled trial. Metabolism. 2013 May;62(5):694–702.
[12] Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7;346(6):393–403. Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006 Sep;29(9):2102–7. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001 May 3;344(18):1343–50. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006 Feb;49(2):289–97. Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract. 2005 Feb;67(2):152–62. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997 Apr;20(4):537–44. Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994 Sep;17(9):961–9. Poulsen P, Kyvik KO, Vaag A, Beck-Nielsen H. Heritability of type II (non-insulin-dependent) diabetes mellitus and abnormal glucose tolerance—a population-based twin study. Diabetologia. 1999 Feb;42(2):139–45.
[13] See Taubes, above, at 5.
[14] Fryar CD, Carroll MD, Ogden CL. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults Aged20 and Over: United States, 1960–1962 Through 2013–2014. Natl Cent Health Stat Health E-Stats. 2016 Jul; Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA. 2015 Sep 8;314(10):1021–9.

