About this Issue
For years, dietary advice held that we should limit our salt, fat, and cholesterol intake. There’s a big problem with that, though: Salt, fat, and cholesterol all to varying degrees either make food taste good, or are found naturally in foods that people enjoy eating. If we’re trying to avoid them, and if the life of an ascetic doesn’t appeal to us, what shall we eat?
The answer was sugar. Sugar also tastes good. For more than a generation, Americans in particular have substituted sugar and other carbohydrates for the fats that they used to consume. They’ve also upped their calorie intake, again largely from sugar. The downsides here seemed few, because dental cavities are not life threatening, and because, although sugary foods may be low in vitamins and other nutrients, most Americans were getting those nutrients elsewhere, making deficiencies relatively rare.
Now, though, scientific opinion has shifted, prompted by two bodies of evidence. First, there has been an epidemic of obesity that seems increasingly to have been the fault of excess sugar consumption. And second, the dietary harms from salt, fat, and cholesterol seem to have been much less than initially feared. Fat does not make people fat — but sugar does, says the new thinking. Sugar also may be to blame for diabetes, heart disease, and a host of other maladies.
The role of government nutrition guidelines looms large in these matters, because these guidelines shape institutional food practices in places like schools, hospitals, and prisons, and because the guidelines shape public health campaigns for the rest of us. Has sugar been making us fat? And if so, has the federal government had a hand in it? And what’s to be done about it?
Joining us to discuss this month are noted science author Gary Taubes, whose lead essay reviews the state of the science and recaps the recent history of U.S. federal government dietary advice. Responding to him are obesity researcher Stephan Guyenet, Professor Yoni Freedhoff of the University of Ottawa, and Professor Terence Kealey of the University of Buckingham. We welcome your comments to their posts and look forward to a stimulating discussion.
Lead Essay
Unintended Consequences, Special Interests, and Our Problem with Sugar
Forty years ago this month, January 1977, the federal government entered the business of giving dietary advice, first with a Congressional report released by George McGovern’s bipartisan Select Committee on Hunger and Human Needs, which in turn prompted the first Dietary Guidelines from the U.S. Department of Agriculture.
With the perfect acuity of hindsight, two stories from those initiatives bear recalling. The first involves McGovern’s report, Dietary Goals for Americans, which was primarily controversial for its recommendation that Americans should reduce the fat content of their diets and compensate with more carbohydrates. After releasing the report, McGovern’s committee held a series of hearings to deal with the backlash, both from scientists and industry. While McGovern, his colleagues, and their committee staff may have all hoped the guidelines would lead to a nation eating, perhaps, as Michael Pollan would later memorably put it, (whole) food, “mostly plants and not too much,” that would not be the case. Hence story number one is about the dangers of unintended consequences.
The Committee’s staff director later told me a story of how he got an inkling of what would eventually happen. As he recalled it, an economist pulled him aside after one of the hearings and gave him a lesson on market disincentives to healthy eating: ”He said if you create a new market with a brand-new manufactured food, give it a brand-new fancy name, put a big advertising budget behind it, you can have a market all to yourself and force your competitors to catch up. You can’t do that with fruits and vegetables. It’s harder to differentiate an apple from an apple.”
And this is indeed what happened. Supermarkets became full of low-fat food products—“foodlike substances,” to borrow again from Pollan—all with implicit or explicit health claims that they would lower cholesterol and bestow a longer and healthier life. Many of these products replaced fat with some variant of the 50-50 combination of glucose and fructose that makes up what we think of as sugar—most notably, high fructose corn syrup, which had just recently entered the food supply. While this transition was occurring, our nation and the world also experienced unprecedented increases in the prevalence of obesity and diabetes, raising the question of whether these two phenomena are causally related.
This brings us to story number two. McGovern’s Dietary Goals prompted Carol Foreman, an assistant secretary of agriculture appointed by President Jimmy Carter, to begin the process of codifying the goals as official government policy. As Foreman later told me, she was aware of scientific controversy on the nature of a healthy diet, but she believed that sufficient consensus existed to provide at least provisional recommendations. “Tell us what you know and tell us it’s not the final answer,” Foreman says would tell nutrition researchers at the time; “tell [us] what your best sense of the data is right now.”
The “best sense of the data,” however, will always depend on who is asked. And therein lies what may be the second problem with the last forty years of dietary guidance in the United States: The existence of a controversy in science implies that uncertainty exists about whether the consensus is correct. Clearly in the 1970s, the majority opinion among nutrition authorities was that dietary fat, particularly saturated fat, caused heart disease, and so probably diabetes and obesity as well. The three disorders are highly associated, suggesting a common cause. Since then, the dietary fat hypothesis has repeatedly failed confirmation in clinical trials, but the strong suspicion remains that fat consumption should be limited; it’s still a foundational assumption about the nature of a healthy diet, if not among public health authorities then among the public whose diet they have been trying to hard to influence.
Another unintended consequence emerged from the official embrace of the dietary fat consensus in the 1970s, however, and this may have had far more profoundly damaging implications. The dietary fat consensus negated the viability of a competing hypothesis that highly processed carbohydrates, and particularly sugars, are the macronutrients to worry about in the American diet. By this thinking, the modern diet damages our health not through cholesterol-related mechanisms (or the presence or absence of vitamins and minerals) but through disruptions of insulin signaling, in which diabetes and so premature death is the end state. Coronary heart disease is a consequence as well.
This hypothesis was actively studied and debated through the mid-1970s, but then it was disassociated from the likely causal link that pointed back to refined carbohydrates and sugar. This disassociation was a casualty of the consensus building of the 1970s, aided and abetted by the sugar industry itself, which was the party with the most to lose in the controversy.
The sugar industry worked diligently beginning in the mid-1960s to help shape the anti-fat consensus and assure that sugar was never perceived as anything more than a source of excess, if empty, calories. As influential nutritionists began to argue in the United States (Jean Mayer at the Harvard School of Public Health) and in the United Kingdom (John Yudkin, founder of the first dedicated nutrition department in Europe) that sugar was a very likely cause of heart disease and diabetes, they were in direct conflict with the great majority who believed fat was the problem. The sugar industry used that conflict to its advantage. It launched a methodical public relations campaign with the goal of assuring that no “confirmed scientific evidence link[ed] sugar” to chronic disease. To do so, it recruited and compensated influential researchers in the anti-fat camp (from Harvard, the University of Minnesota, the University of Washington, and elsewhere) to publish authoritative reviews and a 90-page journal supplement, Sugar in the Diet of Man, that reinforced the message that dietary fat was the problem and sugar was not. These documents played a pivotal role in the FDA’s 1976 preliminary assessment that sugar should retain its status as Generally Recognized as Safe (GRAS). And that decision, along with sugar-industry-funded research and industry-funded researchers, then played the critical role in forming the consensus that sugar was benign.
The first USDA Dietary Guidelines, released in 1980, cautioned against consuming “too much” sugar—a tautological statement that could apply to any food. They also stated that “too much sugar does not seem to cause diabetes,” acknowledging the possibility and some controversy. In 1985, the second edition of the Guidelines dropped the conditional and proclaimed unambiguously “too much sugar in your diet does not cause diabetes.” Worth noting is that much of the relevant research done on this question between 1980 and 1985 was carried out at the USDA’s own Carbohydrate Nutrition Laboratory, and the researchers involved vehemently disagreed with this conclusion. By then, though, researchers studying the question of sugar and health were already tarred with the perception of having crossed the line from legitimate science to quackery.
In 1986, the FDA officially concluded that sugar should retain its GRAS status on the basis that “no conclusive evidence demonstrates a hazard to the general public when sugars are consumed at the levels that are now current.” Seminal government reports that followed – from the Surgeon General’s Office (1988), the National Academy of Sciences (1989) and the British Committee on the Medical Aspects of Food Policy (1989) – all echoed this thinking. Dietary fat is a killer; sugar is a benign source of empty calories. To come to the latter conclusion, though, required that the authors of these reports equate “no conclusive evidence” with no evidence at all.
By doing so, they successfully transformed a consensus of opinion into dogma. Among the consequences may have been the worldwide epidemics of obesity and diabetes. Had the nutrition research community and the public health authorities in the 1970s and 1980s understood that scientific controversy can only be resolved by careful experiment, not the assignment of truth to a consensus, then both our medical and public health approaches to obesity and diabetes might have had some effect. We cannot say. Should they understand it now, as I would hope to be the case, we’re still looking at perhaps 20 years of concerted research before definitive answers can be obtained. As such, we’re still in the position of the USDA in the late 1970s, having to act on incomplete and uncertain information, and still left having to make difficult decisions about who has the best sense of the data.
At the core of this kind of nutrition controversy is a fundamental philosophical conflict between the requirements of an effective public health policy and the requirements of science. The belief that imminent action must be taken, that it would in fact be irresponsible not to act, may be incompatible with the institutionalized skepticism and rigor required to establish reliable knowledge. The urgency required to prevent imminent deaths can mean that public health authorities do not have the time to gather what they would often describe to me in my research as “definitive scientific evidence,” sometimes perceived naively as dotting the i’s and crossing the t’s.
Good scientists will argue that the absence of definitive scientific evidence means that the truth remains unknown and, therefore, so does any clearly beneficial path of action, one with minimal and acceptable risks. Science is about acknowledging uncertainty. Effective public health policy requires that the public be convinced to change their behavior for their own good, which requires that we believe such a change is based on the strongest possible evidence. These perspectives may be right in their particular fields of application, but they can also be mutually exclusive. In 1999, when I first began investigating these controversies for the journal Science, the then director of the NIH’s office of disease prevention, William Harlan, captured the conflict this way: “We’re all being pushed by people who say, ‘Give me the answer. Is it or isn’t it?’ They don’t want the answer after we finish a study in five years. They want it now. No equivocation … [And so] we constantly get pushed into positions we may not want to be in and cannot justify scientifically.” A former director of the Center for Food Safety and Applied Nutrition at the FDA put it even more simply: “science,” he said, “is a destabilizing force in public policy.”
While the obesity and diabetes epidemics have finally motivated authorities, most notably the WHO, to advocate limited consumption of sugary beverages, they still do so based on the thinking that the sugar in these beverages provides only empty calories consumed in excess. As such, we’re back to the USDA’s admonishment from 1980: Avoid “too much sugar” and all will be well enough.
The minority opinion is much the same as it was forty years ago: sugar is far worse than a benign source of empty calories. It’s a toxin, albeit not a quick-acting toxin, but one that does its damage over years and decades. It may be the primary cause of diabetes, independent of its calories, and perhaps of obesity as well. If we didn’t consume sugar, by this thinking, both obesity and diabetes would be relatively rare conditions, just as lung cancer would be in the absence of cigarettes.
Another fact that has to be considered when institutions transform a consensus into a dogma is that reliable science not only should move slowly, but inevitably it does. The notion that sugar is a toxin is based on a scientific understanding that was evolving from the 1960s onward. It did so without the attention given to the also evolving research on dietary fat, cholesterol, and heart diseases. When the FDA, USDA, and other organizations embraced the dietary fat consensus, this research and its implications was still virtually unknown to those involved. Its transition to reliable textbook science only began afterward. Only with the full awareness of the obesity epidemic that emerged in the late 1990s have the broader public health implications of this research come to be partially embraced, but by then these new implications had to be reconciled with the assumption that dietary fat is the real problem.
The sugar hypothesis is based on the fact that the fructose component of sugar (and high fructose corn syrup) is metabolized primarily in the liver, resulting in a chain of effects that is speculative but still compelling: first the liver converts the fructose into fat, and that fat accumulates in liver cells (hence a condition, now also epidemic, known as non-alcoholic fatty liver disease). This in turn results in a condition called insulin resistance, which is the fundamental defect in type 2 diabetes. And that insulin resistance is accompanied by a cluster of metabolic abnormalities (high blood pressure, low HDL cholesterol, glucose intolerance) that is now known as metabolic syndrome. It can be thought of as a pre-diabetic condition and is so strongly associated with obesity that it may play a causal role there as well. (The first symptom that a physician is instructed to look for in diagnosing metabolic syndrome is increasing central adiposity – i.e., the patient is getting fatter) The CDC estimates that 75 million Americans have metabolic syndrome. Insulin resistance and metabolic syndromes are powerful predictors of heart disease. So the assumption is that what causes one, causes all. Most authorities believe that metabolic syndrome, like obesity, is caused by excess calories – eating too much and sedentary behavior. Experiments in both animals and humans suggest that sugar-rich diets should be at least a prime suspect.
If sugar consumption does cause insulin resistance and metabolic syndrome, then the dietary prescriptions of the past forty years are tragically incorrect. The question is what we can do about it now, when the evidence is still ambiguous and when the sugar-is-toxic camp is still very much a minority. The research necessary to nail it down would take years to decades to complete and is not even on the radar screen of the funding agencies.
Once again we’re in the position of having to take action based on uncertain evidence amid what is now a public health crisis. The twin epidemics of obesity and diabetes worldwide are a “slow-motion disaster,” in the words of Margaret Chan, director general of the World Health Organization. Chan gave a keynote address at an October meeting of the National Academy of Medicine and predicted with virtual certainty that the situation would continue getting worse for the foreseeable future.
Whatever actions we take, though, are like to have unintended consequences. One of them is further ingraining the precedent for taking other actions that are likely to be wrong and damaging as well. Clearly rigorous research is necessary to clarify the inherent uncertainty in the nature of a healthy diet and specifically the role of sugar in human health and disease. We have to know beyond reasonable doubt the dietary triggers of obesity and diabetes. If sugar plays a unique role, then we have to act. But that research will take time and a concerted effort that is not even on the radar screen of the National Institutes of Health. If that research is guided by the same influential authorities who have overseen the last forty years of dietary guidance and the epidemics of obesity and diabetes coincident with them, and if that thinking is indeed wrong, further errors are likely to be propagated.
If this were any other crisis, if this were any other public health failure, we would be assembling task forces of unbiased, independent researchers, perhaps from outside the field if necessary, to rigorously assess the evidence, determine what errors have indeed been made, and decide what to do next. It’s the only solution I can see to an intractable problem.
Response Essays
Americans Eat Too Much Cake, but the Government Isn’t To Blame
Gary Taubes paints a lively picture of lawmaker overzealousness, industry subterfuge, and researcher bias to argue that fat may have been unfairly blamed for the ravages of sugar, and as a result, misguided government dietary advice drove Americans to eat more sugar, ultimately contributing to obesity, diabetes, and coronary heart disease. Yet the key questions Taubes raises cannot be evaluated via historical narrative. It’s time to hang up our tweed blazers and slip into our white lab coats, because Taubes has made specific and testable assertions, which I will evaluate in three parts. First, I will examine the 1980 Dietary Guidelines to determine if they condemn fat and take a weak stance on sugar as suggested. Second, I will evaluate the hypothesis that the Guidelines contributed to obesity, diabetes, and coronary heart disease. And third, I will evaluate the hypothesis that sugar “may be the primary cause” of the three aforementioned conditions.
Inside the 1980 Dietary Guidelines for Americans
In the opening sentence of his essay, Taubes states that “forty years ago this month, January 1977, the federal government entered the business of giving dietary advice,” referring to a congressional report that gave rise to the 1980 Dietary Guidelines for Americans. In fact, the federal government has been issuing dietary advice regularly for over a century.[1] The 1980 Guidelines were, however, notable for the fact that they abandoned the traditional “eat more” approach of diversifying and balancing the diet, in favor of an “eat less” approach of limiting foods perceived as unhealthy.[2]
Taubes argues that this document condemned fat and took a weak stance on sugar. Let’s have a look for ourselves.[3] At the core of the 1980 Guidelines were seven pieces of dietary advice, shown below:
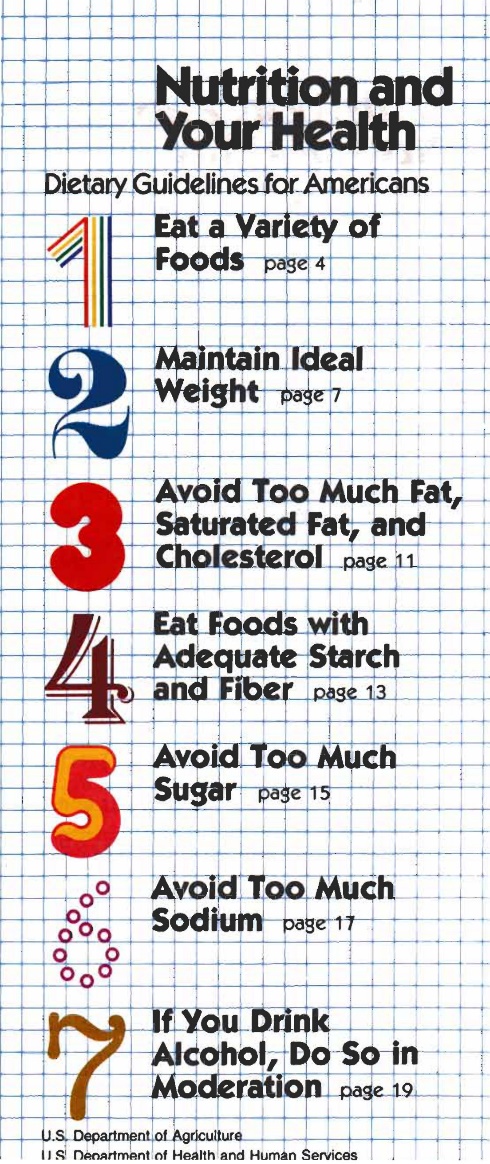
As you can see, “avoid too much fat” and “avoid too much sugar” are equally prominent and identically worded recommendations. Taubes suggests that the statement “avoid too much sugar” is vague and lacks conviction—it is “a tautological statement that could apply to any food.” Yet we are intended to believe that the same language applied to fat altered the course of the American diet.
The Guidelines went further, providing explicit guidance on how to “avoid too much sugar”:
- Use less of all sugars, including white sugar, brown sugar, raw sugar, honey, and syrups.
- Eat less of foods containing these sugars, such as candy, soft drinks, ice cream, cakes, cookies.
In the section titled “Maintain Ideal Weight,” the document lays out its four-part plan for weight loss: Increase physical activity, eat less fat and fatty foods, eat less sugar and sweets, and avoid too much alcohol. Again, the advice to limit fat and sugar intake receive equal attention, and the Guidelines clearly implicate excess sugar intake in obesity.
A person who faithfully adhered to the Guidelines would end up eating a diverse, largely unprocessed diet composed of whole grains, beans, nuts, lean meats, seafood, dairy, eggs, vegetables, and fruits, with little added sugar, added fat, or highly processed foods or beverages. Are we really to believe that this advice—which clearly and repeatedly recommended eating less sugar—made Americans eat more sugar, leading to obesity, diabetes, and coronary heart disease? Having reviewed the Guidelines, the notion strains credulity, but let’s test it anyway.
Wrath of the Guidelines
Taubes argues that the Guidelines may have unintentionally contributed to obesity, diabetes, and coronary heart disease. This rests on the assumption that the Guidelines themselves substantially influenced American eating behavior, either directly or indirectly via the food industry, and therefore that changes in the American diet over time can be attributed to it rather than to the numerous other shifts in the American food and cultural landscape that were happening at the time.[4] No evidence is presented to support this assumption, so we will examine it here.
If the Guidelines substantially influenced the American diet, then we should observe that total fat, added fat, and added sugar intake declined in its wake. In perfect contrast to this prediction, our total intake of fat remained approximately the same after the Guidelines, our intake of added fat increased, and our intake of added sugar increased.[5],[6]
Furthermore, we should observe a decline in the consumption of highly processed foods rich in fat and sugar that the Guidelines clearly advised against. To test this prediction, here are the top six sources of calories in the U.S. diet, in descending order of importance, as of 2006:
- Grain-based desserts (cakes, cookies, donuts, pies, and related items)
- Yeast breads
- Chicken and chicken-mixed dishes
- Soda, energy drinks, and sports drinks
- Pizza
- Alcoholic beverages[7]
This list is both disturbing and informative. Cake and related desserts are the number one source of calories in the American diet. Soda, pizza, and alcohol are three of the remaining five items. The average American diet is not even remotely inspired by the Guidelines.
The truth is that we don’t wash down our pizza and cake with beer and soda because we think it’s healthy or because we believe the government recommended it. We do it because we are human beings who are driven by considerations of pleasure, cost, and convenience—precisely the qualities the food industry has been optimizing for the last 40 years.[8]
Taubes assumes that we suffer from increasing rates of obesity and diabetes because we have failed to identify their true cause. Yet the evidence suggests a simpler and more compelling explanation: We eat too much food that is obviously unhealthy, and it’s not because researchers or the government told us to, but because we like it.
A Slow-Acting Toxin
According to Taubes, sugar may be a “toxin” and “the primary cause of diabetes, independent of its calories, and perhaps of obesity as well.” Elsewhere in the essay, coronary heart disease is added to the list. Yet Taubes asserts that this speculative hypothesis cannot currently be tested because there is so little existing research on sugar, and so little interest in conducting such research, that “the research necessary to nail it down would take years to decades to complete and is not even on the radar screen of the funding agencies.”
This belief is remarkable in light of the fact that a Google Scholar search returns hundreds of scientific papers on the health impacts of sugar, many of them human randomized controlled trials, and many funded by the U.S. National Institutes of Health. In reality, the health impacts of sugar are of considerable interest to the scientific community, and as such, they have been studied extensively. Having established that this research exists, let’s take a look at it.
The hypothesis that sugar is the primary cause of coronary heart disease is easily refuted. In the United States, coronary heart disease mortality has plummeted by more than 60 percent over the last half century, despite a 16 percent increase in added sugar intake.[9] Roughly half of this decline can be attributed to better medical care, while the other half is attributed to underlying drivers of disease such as lower cholesterol and blood pressure levels and an impressive drop in cigarette use.[10]This striking inverse relationship is incompatible with the hypothesis that sugar is the primary cause of coronary heart disease, although it doesn’t exonerate sugar.
Is sugar the primary cause of diabetes, “independent of its calories”? Research suggests that a high intake of refined sugar may increase diabetes risk, in large part via its ability to increase calorie intake and body fatness, but it is unlikely to be the primary cause.[11] An immense amount of research, including several large multi-year randomized controlled trials, demonstrates beyond reasonable doubt that the primary causes of common (type 2) diabetes are excess body fat, insufficient physical activity, and genetic susceptibility factors.[12]
The ultimate test of the hypothesis that sugar is the primary cause of obesity and diabetes would be to recruit a large number of people—perhaps even an entire country—and cut their sugar intake for a long time, ideally more than a decade. If the hypothesis is correct, rates of obesity and diabetes should start to decline, or at the very least stop increasing. Yet this experiment is far too ambitious to conduct.
Or is it? In fact, this experiment has already been conducted—in our very own country. Between 1999 and 2013, intake of added sugar declined by 18 percent, taking us back to our 1987 level of intake. Total carbohydrate intake declined as well.[13] Over that same period of time, the prevalence of adult obesity surged from 31 percent to 38 percent, and the prevalence of diabetes also increased.[14]
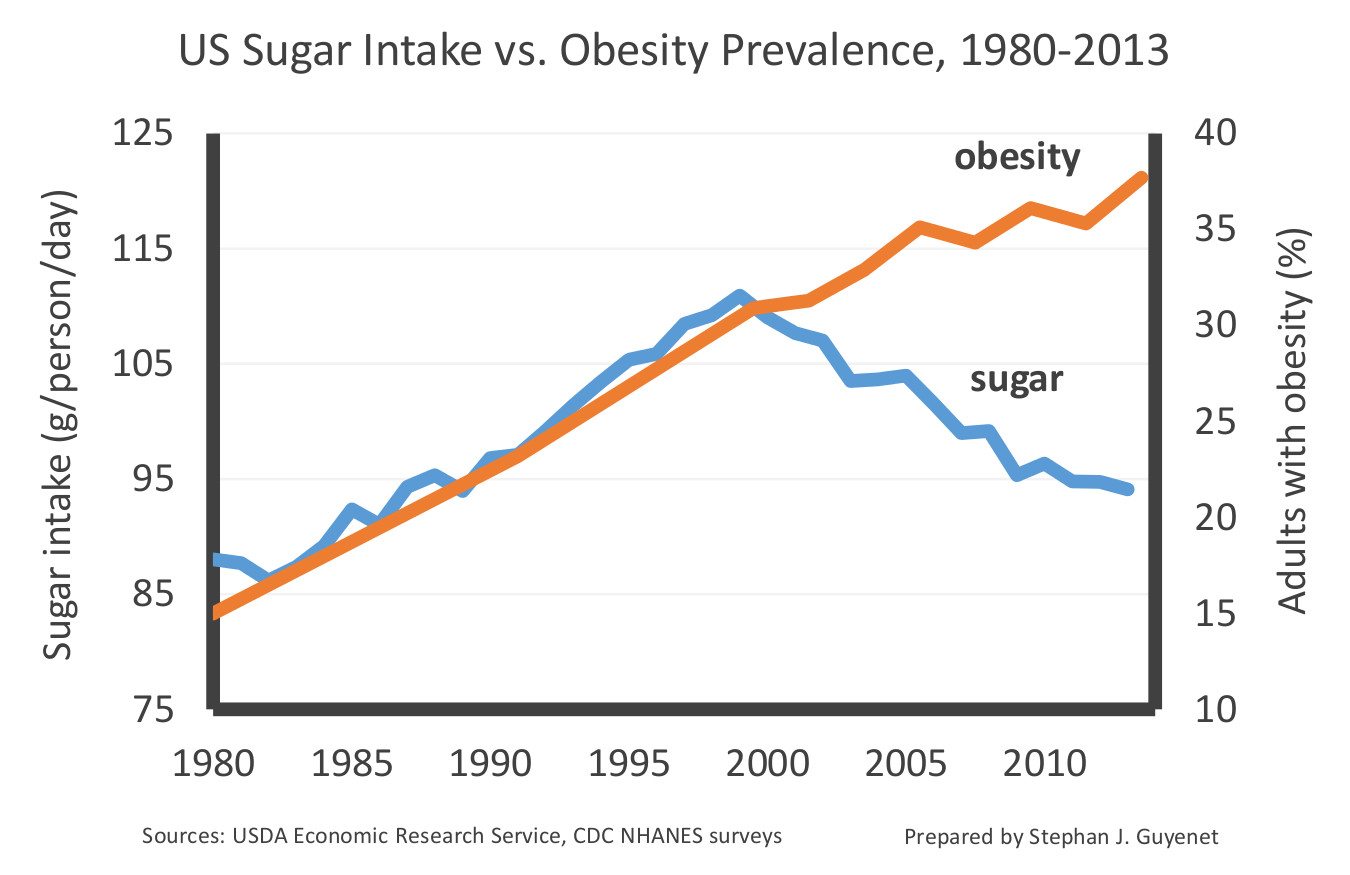
U.S. sugar intake and adult obesity prevalence, 1980-2013. Data are from Centers for Disease Control and Prevention NHANES surveys and USDA Economic Research Service food disappearance records (5,6). Axes are bounded to illustrate correlation, or lack thereof.
Americans have been reining in our sugar intake for more than fourteen years, and not only has it failed to slim us down, it hasn’t even stopped us from gaining additional weight. This suggests that sugar is highly unlikely to be the primary cause of obesity or diabetes in the United States, although again it doesn’t exonerate sugar. Furthermore, it suggests that the laser-like focus on sugar is a distraction from the true, more complex nature of the problem.
I have presented a small piece of a large body of evidence that is more than sufficient to refute the assertion that sugar may be the primary cause of obesity, diabetes, and coronary heart disease. At the same time, this evidence does suggest that added sugar is part of a broader diet and lifestyle landscape that contributes to these three conditions, a conclusion that is not especially controversial within today’s scientific, medical, and public health communities.
[1] Davis C, Saltos E. Dietary Recommendations and How They Have Changed Over Time. USDA Economic Research Service; 1999.
[2] Nestle M. Food Politics: How the Food Industry Influences Nutrition, and Health, Revised and Expanded Edition. Berkeley: University of California Press; 2007. 510 p.
[3] Nutrition and Your Health. Dietary Guidelines for Americans. US Department of Agriculture and US Department of Health and Human Services; 1980.
[4] For example, the declining cost of sweeteners and processed food in general, increasing ubiquity of food and advertising, advances in food sensory engineering, and the replacement of home cooking with restaurant and pre-prepared food. I discuss these trends in my book The Hungry Brain.
[5] Taubes has previously argued that the percentage of fat in the U.S. diet declined in the wake of the Guidelines, which is correct. However, this percentage change was due to an absolute increase of carbohydrate intake, not an absolute decline of fat intake. Since our absolute intake of fat remained unchanged, this cannot be interpreted as a decline of fat intake. USDA Economic Research Service - Food Availability (Per Capita) Data System [Internet]. 2016 [cited 2016 Dec 22]. Available from: https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/. Austin GL, Ogden LG, Hill JO. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971-2006. Am J Clin Nutr. 2011 Apr;93(4):836–43.
[6] Throughout this piece, the term “added sugar” refers to table sugar, high-fructose corn syrup, honey, and all other calorie-containing sweeteners, including both home use and consumption via prepared foods and beverages. It does not include the sugar naturally found in fruit, vegetables, and milk.
[7] U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. U.S. Government Printing Office; 2010.
[8] Moss M. Salt Sugar Fat: how the food giants hooked us. New York: Random House; 2013.
[9] Ibid. See also USDA, above, and Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004 Aug 3;110(5):522–7. And Ford ES, Roger VL, Dunlay SM, Go AS, Rosamond WD. Challenges of ascertaining national trends in the incidence of coronary heart disease in the United States. J Am Heart Assoc. 2014 Dec 3;3(6):e001097.
[10] Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007 Jun 7;356(23):2388–98.
[11] Horst KW ter, Schene MR, Holman R, Romijn JA, Serlie MJ. Effect of fructose consumption on insulin sensitivity in nondiabetic subjects: a systematic review and meta-analysis of diet-intervention trials. Am J Clin Nutr. 2016 Dec 1;104(6):1562–76. Black RNA, Spence M, McMahon RO, Cuskelly GJ, Ennis CN, McCance DR, et al. Effect of eucaloric high- and low-sucrose diets with identical macronutrient profile on insulin resistance and vascular risk: a randomized controlled trial. Diabetes. 2006 Dec;55(12):3566–72. Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009 May;119(5):1322–34. Lewis AS, McCourt HJ, Ennis CN, Bell PM, Courtney CH, McKinley MC, et al. Comparison of 5% versus 15% sucrose intakes as part of a eucaloric diet in overweight and obese subjects: effects on insulin sensitivity, glucose metabolism, vascular compliance, body composition and lipid profile. A randomised controlled trial. Metabolism. 2013 May;62(5):694–702.
[12] Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7;346(6):393–403. Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006 Sep;29(9):2102–7. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001 May 3;344(18):1343–50. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006 Feb;49(2):289–97. Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract. 2005 Feb;67(2):152–62. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997 Apr;20(4):537–44. Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994 Sep;17(9):961–9. Poulsen P, Kyvik KO, Vaag A, Beck-Nielsen H. Heritability of type II (non-insulin-dependent) diabetes mellitus and abnormal glucose tolerance—a population-based twin study. Diabetologia. 1999 Feb;42(2):139–45.
[13] See Taubes, above, at 5.
[14] Fryar CD, Carroll MD, Ogden CL. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults Aged20 and Over: United States, 1960–1962 Through 2013–2014. Natl Cent Health Stat Health E-Stats. 2016 Jul; Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA. 2015 Sep 8;314(10):1021–9.
Unintended Consequences, Special Interests, Sugar, and a View from the Clinical Trenches
If in 1977 Americans had actually followed McGovern’s 7 dietary recommendations, they’d likely be a lot better off today. Though McGovern’s recommendations did indeed call for increasing dietary carbohydrates, they recommended their increase come from fruits, vegetables, and whole grains, not Wonder Bread, Froot Loops, and Coca-Cola. They also recommended decreasing red meat consumption in favor of fish and poultry, that poly-unsaturated fats replace saturated, and with their admonishment to limit foods high in salt, sugar, and fat, they effectively recommended that the public shy away from ultra-processed foods – foods which tend to use one or more of those ingredients to create the “bet you can’t eat just one” phenomenon of hyper-palatability.
Pertinent to this discussion, the guidelines also expressly called for a drastic reduction in sugar, recommending it account for no more than 10% of Americans’ total daily energy intakes. (But they did likely get eggs wrong – the evidence suggesting that there’s real benefit to limiting dietary sources of cholesterol hasn’t stood time’s test.)
Taubes asserts that America’s dietary guidelines, starting with McGovern’s purported low-fat call to arms, led to fat’s unintended dietary replacement with sugar and simple carbohydrates. Whether it’s fair to call America’s current dietary woes the “unintended consequence” of not actually following recommendations that also explicitly called for a severe reduction in dietary sugar and ultra-processed foods, there’s no disagreement that the guidelines were not followed. And while a diet that provides 30% of calories from fat, as McGovern’s recommended diet did, isn’t fairly describable as a low-fat diet, Taubes’ point that over-simplified messages risk unintended consequences is an important one – and one we should be reminded of when we see headlines suggesting butter to be not just benign but rather a health food.
Truth be told, despite the inference that Americans replaced dietary fats with simple carbohydrates and sugars, the data would suggest that Americans consume just as much fat as they always did – it’s just that they’re consuming more of everything else. While the percentage of a person’s daily energy intake coming from dietary fat has indeed dropped, the absolute amount of dietary fat being consumed hasn’t changed since at least the very early 1970s.
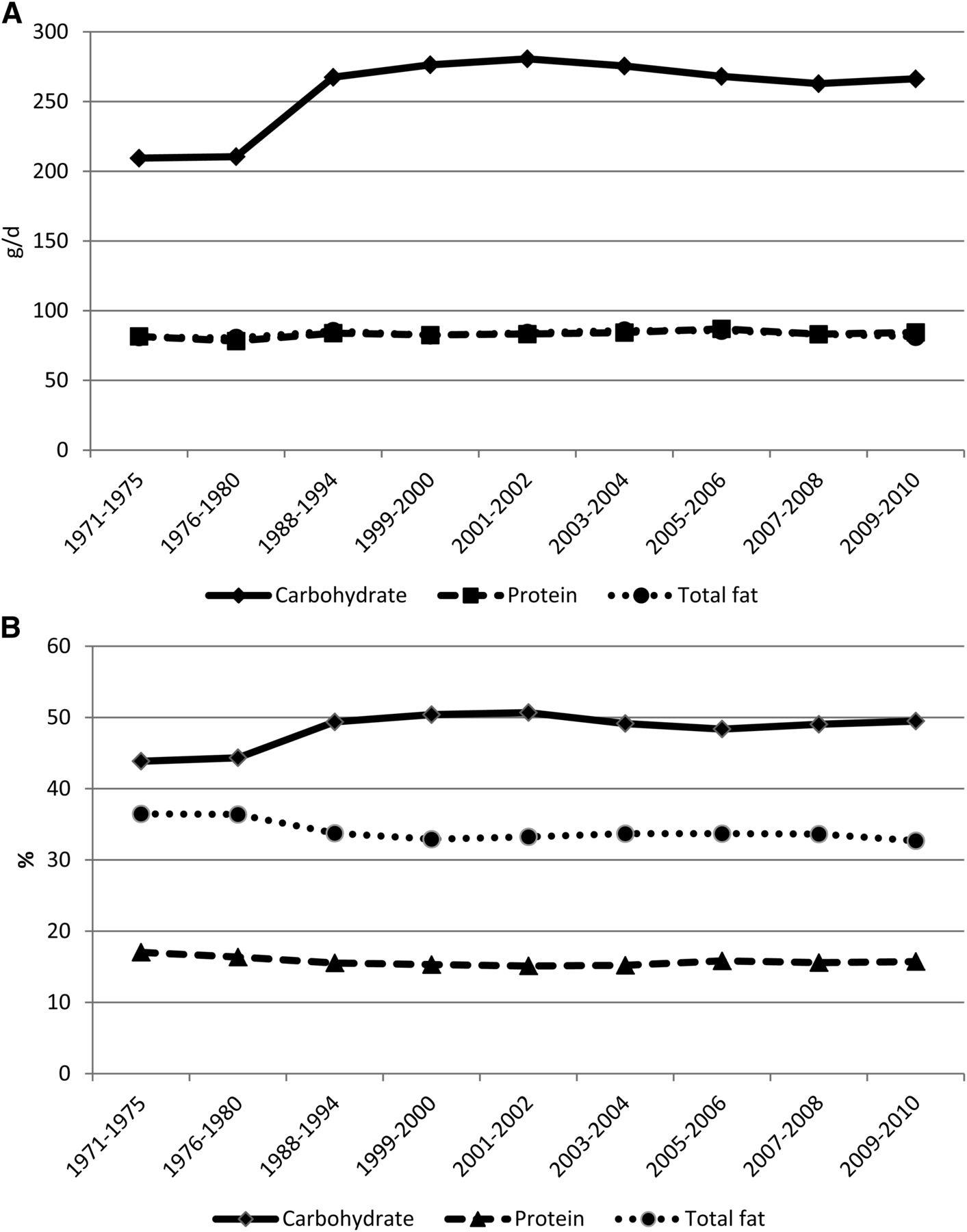
Figure 1: Mean adjusted intakes of macronutrients among adults aged 20–74 y by NHANES study period. A: Results shown as absolute intake in grams per day. B: Results shown as percent of total intake.
Or hasn’t it?
Unfortunately, we don’t have great dietary consumption data to draw upon. Instead we’re left to expound on studies reliant on food frequency questionnaires, which in turn have been shown to be extremely unreliable. One recent scathing review of the use of dietary recall and food frequency questionnaires asserted that their use was “akin to creation science in that they fail to meet the basic requirements of scientific research.
So while it’s fair to point out the flaws in the science that built the case against dietary fats in the 70s and 80s, it’s also fair to point out that there are flaws as well in building the case against sugar, as those who are building it can’t help but also use much of that same challenged pool of dietary evidence. Worse, we may never have the means with which to determine truly specific causal factors when it comes to diet and health, and that’s not even considering the incredible number of confounders that freely living human populations possess. For example, even in captive populations of genetically identical mice fed tightly restricted and controlled diets, there are dramatic confounders, whereby a captive mouse’s living arrangements (eg. noise, bedding, light, the pH of their water, the microbiome prevalent from each particular vendor’s mice, fecal oral eating, and more) have been shown to markedly affect study outcomes, including their metabolic responses to identical diets.
This all helps to explain why Taubes’ assertion that “[t]he ‘best sense of the data,’ however, will always depend on who is asked” rings so true. With decades of food frequency questionnaires informing hundreds if not thousands of studies, and given the degree of confounding that exists from person to person let alone from nation to nation, there is something for everyone in the scientific literature. And given no one is free from confirmation and intellectual sunk cost biases, cherry picking to make the case against fat or sugar is neither difficult nor surprising to see.
What’s also not surprising is that there are scads of conflicts of interest in nutrition. Dietary recommendations are big business for the food industry, while recommending diets is big business for publishing. The weight loss industry has been reported as being a $60 billion per year juggernaut in North America alone, and that doesn’t include the dollars involved in the pursuit of different dietary strategies selling health (which would include such things as organics, GMOs, gluten, and other dietary recommendations and fads).
Taubes’ work compellingly cultivates concerns about the many conflicts of interest inherent to nutrition science. It’s important though to note that financial conflicts with the food industry have never been shown to be uniquely influential among all financial conflicts. Equally worthy of consideration are funding by nonprofits with established and specific points of view, as well as of course personal profit – where some have translated their take on nutrition science into massive book and speaking deals. So while Taubes justly notes that sugar science is speculative, unambiguous statements and cherry picked data are certainly not exclusive to the public discourses of nutrition researchers about dietary fats.
Conflicts aside, there’s no denying the rise of chronic, non-communicable diseases (NCDs) since the McGovern era. So where to lay blame? Well, we’re definitely eating more. Portion sizes have grown, both in our homes and when eating out. We’re spending 18 times as much money as we once did in restaurants. We’re purchasing twice as much processed food and sweets as we did in the 80s. The Don Drapers of the real world command multi-billion dollar junk food marketing budgets, and are spending – this is not a typo – 150 times more than in the 80s, to specifically target children. Our teachers, coaches, and camp counselors use junk food to reward, pacify, and entertain our kids at nearly every turn. And there seems to be no occasion too small to not warrant celebrating it with junk food. And it’s not just that we’re eating too much, what we’re eating is a mess.
Studies conducted in developing nations show the rise of NCDs to proceed in near lockstep with the introduction of a so-called westernized food supply. Our best evidence currently points to ultra-processed foods as the causal culprits, with a basic definition of ultra-processed being:
Ready to consume (or heat) formulations manufactured from cheap ingredients either directly extracted from whole foods or processed from components extracted from whole foods (e.g. high-fructose corn syrup). These products typically contain the addition of preservatives and “cosmetic additives” and are usually energy dense with high fat, sugar, and salt contents and with little or no water, fibre, micronutrients, or other “protective bioactive compounds” which exist in whole foods.
We don’t fully know what it is about ultra-processed foods that leads them to be so tightly linked to NCDs including obesity and diabetes. While the prospect of a single, causal, Occam’s razor-esque nutrient to blame is both seductive and hopeful, science has not clearly identified one. Loss-adjusted food availability data, bolstered by documented portion size and spending pattern changes, offers more objective data than dietary recall surveys, but at this point such studies only clearly finger our eating much more than we ever did. That said, there’s no doubt sugar is a major raindrop in our flood of excess calories, serving as one of the primary drivers of hyper-palatability, as well as a key ingredient in a large percentage of likely less sating, ultra-processed foods, and especially of the sugar-sweetened beverages of which we’re drinking a great deal more.
Discussions of which nutrient to blame may further confuse an issue that doesn’t benefit from the confusion, especially when viewed from the clinical trenches. While Taubes feels very strongly about knowing “beyond reasonable doubt” the triggers of obesity and diabetes, and the specific role of sugar in human health and disease, and putting aside the possibility that sometimes multiple roads lead to the same destination, as someone whose full time daily job for the past 13 years has been to work with individuals on improving their lifestyles, I think that looking only to sugar misses the forest for the trees when it comes to helping people to improve their health.
As a clinician with a full time behavioral weight management practice, and as a fierce public health policy critic, I believe that pragmatism and realism are more important than idealism and rigidity in cultivating behavior change. While I would readily agree with Taubes that sugar reduction is a very worthy goal, as a goal it’s simultaneously not enough, and too much. It’s not enough as there are many other actionable areas ripe for behavior changes which if enacted would markedly reduce a person’s risk of developing NCDs, and it’s too much in that with food certain to forever serve all of us in roles of both comfort and celebration, sugar’s singular demonization, if embraced, may lead to calls for extremes of action that even if enacted, aren’t likely to be enjoyable enough to be sustainable for most.
History also informs us of the risks of single-nutrient battle cries. The excessive amplification of “low-fat” messages enabled the sale, and likely encouraged the consumption, of ultra-processed low-fat foods. With this as our backdrop, let’s hope that public health policy makers heed Taubes’ warning that,
Whatever actions we take, though, are likely to have unintended consequences. One of them is further ingraining the precedent for taking other actions that are likely to be wrong and damaging as well.
We should offer diet guidance far more broadly than just on sugar so as not to unintentionally fuel a surge in the manufacture and consumption of new low-sugar ultra-processed foods. There are incredible health benefits to be had from looking at broad based behaviors; an emphasis on sugar alone might overlook them. Behaviors such as:
- Cooking meals from fresh whole ingredients while minimizing restaurant meals and ultra-processed foods; eating those meals free from distractions, and ideally with friends or family.
- Exercising as often and as much as is enjoyable, and appreciating that short bouts also provide benefit.
- Not smoking.
- Cultivating good night sleeps.
- When considering any dietary indulgence, asking first if it’s worth it, and second, if it is, what’s the smallest amount needed to be happy?
- Drinking alcohol only in moderation.
- Nurturing friendships and relationships.
This sort of back to basics approach is what underlies Brazil’s recently published and highly praised dietary guidelines, where rather than try to distill divergent, challenged, and often conflicted studies into a set of highly specific recommendations, their aim was to encourage much broader patterns of healthy eating and living. Were Americans as a whole to adopt even just the aforementioned 7 behaviors, not only would their sugar intake be reduced, but so too would the burden of many NCDs.
Lastly, while Taubes believes that “Effective public health policy requires that the public be convinced to change their behavior for their own good,” it’s important to remember that behavior change for one’s own good may be an unrealistic luxury for many. Instead effective public health policy requires that the public be guided to behavior change by way of an environment designed to make health enriching choices easier, cheaper, and/or unavoidable.
Putting Nutrition Claims to the Test
Gary Taubes has been the most influential voice in nutrition since Ancel Keys, but since Keys is now universally excoriated, that may not be an unmitigated honor: how do we know that Taubes is not as flawed? It is certainly unprecedented for the most influential voice of a major scientific discipline, in this case nutrition, to be a journalist rather than a scientist, but since Keys was a scientist, perhaps nutrition does need to be led by a non-scientist. Let’s see.
Between 1953 and 2002, the world of nutrition was dominated by Ancel Keys’s hypothesis that heart attacks and strokes were caused by an excess of fat in the diet,[1] but in 2002 Taubes wrote an article in the New York Times Magazine “What if It’s All Been a Big Fat Lie?” that almost overnight converted the nutritional avant garde from fat-phobia to carbohydrate-phobia.[2] Taubes went on to expand his article into the best-selling 2007 book Good Calories, Bad Calories.[3]
Taubes, a physicist who became a science journalist, has made a career of exposing poor research. To expose the brutal politics within the world of high-energy physics, he subtitled his first book Nobel Dreams (1986) as Power, Deceit and the Ultimate Experiment. In 1993 he published his second book, Bad Science: The Short Life and Weird Times of Cold Fusion, to analyze the failings of the Fleischmann-Pons experiment. Having eviscerated physics, Taubes moved on to nutrition because, in his words, “I had a lot of people in the physics community say to me that if I was interested in bad science I should look at this stuff in public health because that is really bad.”[4]
So, what is Taubes’s difficulty with the Keys fat hypothesis? Keys (1904–2004) of the University of Minnesota faced the problem, as did all of America in the 1950s, of the sudden epidemic of heart attacks. Frighteningly, these had seemingly come out of nowhere. Absence of evidence is not evidence of absence, but in a study published in the British Heart Journal Leon Michaels, a Canadian physician, showed that the absence of evidence for heart attacks before the 20th century was indeed evidence for their absence.[5] Cleverly, Michaels compared the characteristic chest pain of heart attacks with the characteristic pain and symptoms of migraine and gout, showing that whereas frequent descriptions of migraine and gout can be found in medical texts from all eras, stretching back to Greek and Roman times, angina and heart attacks started to be described with any frequency only in the 20th century: heart attacks really were a new disease, yet a plague of them had descended on the United States like avenging angels, and by midcentury they had become by far the commonest cause of death. Nor were they respecters of persons: President Eisenhower had a heart attack in 1955, while Franklin Roosevelt had died from the related condition of stroke.
Heart attacks and strokes are caused by atherosclerosis, which used to be known as “hardening” of the arteries but which is better described as “inflammation” of the arteries. By Keys’s day it seemed clear that atherosclerosis, in its turn, was caused by the deposition of cholesterol in the arteries, and since people with heart attacks had raised levels of cholesterol in the blood, and since eating an excessive amount of saturated fat raised the blood levels of cholesterol, it seemed obvious that cutting back on fat in the diet would help prevent heart attacks and their related condition of strokes.
And it did! Contrary to myth – a myth to which Taubes himself has contributed – the course of the heart attack epidemic in America followed the Keys fat paradigm almost faultlessly. So between 1960 and 2000 the per capita U.S. consumption of
- saturated fatty acids fell from 55 to 46 grams per day
- cholesterol fell from 465 to 410 milligrams per day.
Meanwhile the per capita U.S. consumption of
- carbohydrates rose from 380 to 510 grams per day
- fiber rose from 18 to 26 grams per day.[6]
And at the same time, the incidences of heart attacks and strokes in America … collapsed! So between 1970 and 2010 the heart attack rate fell by 75 per cent (i.e., in 2010 it was only a quarter of the rate in 1970) while the stroke rate fell markedly too.[7] Has Keys not been exonerated and Taubes disproved by these data? And with that extraordinary public benefit, need we worry about a bit of diabetes and a touch of obesity? These are, after all, apparently translating into a remission of the epidemic of heart disease.
I am of course writing that penultimate sentence ironically. The facts are unambiguous, but the truth – as Taubes himself acknowledges – is that we still don’t know what has caused the remission in heart disease nor the current epidemics in obesity and type 2 diabetes. Taubes blames the latter on sucrose, but I think the case is not yet proven – and indeed neither does Taubes, hence his wonderful initiative in creating with Dr. Peter Attia the Nutrition Science Initiative (NuSI) to study health to the highest standards of scientific objectivity.
As his essay demonstrates, Gary Taubes deservedly remains the most influential person in nutrition today, not only because he smashed the fat consensus, and not only because he has recognized the metabolic syndrome as the greatest health threat facing the western world today, but also because he is honest enough to know that even his own faith in the sugar hypothesis needs dispassionate testing. Moreover, in his defense of science as a process that must be freed from government demands for immediate results, he has shown he understands the scientific method better than many a practicing nutritional researcher.
Notes
[1] A Keys (1953) Atherosclerosis: A problem in newer public health. Journal of the Mount Sinai Hospital 2: 118-139.
[2] G Taubes (7th July 2002) “What if It’s All Been a Big Fat Lie?” New York Times Magazine.
[3] G Taubes (2007) Good Calories, Bad Calories Knopf NY.
[4] Quoted by B Appleyard (1 January 2017) How sugar got us in a sticky mess. Sunday Times Magazine, p 24-27.
[5] L Michaels (1966) Aetiology of coronary heart disease: An historical approach. Br Heart J 28: 258-264.
[6] S-S Zhou et al (2010) B-vitamin consumption and the prevalence of diabetes and obesity among US adults: population based ecological study. BMC Public Health 10: 746. www.biomedcentral.com/1471-2458/10/746
[7] A Statement from the American Heart Association/American Stroke Association (2013) Factors Influencing the Decline in Stroke Mortality. https://professional.heart.org/idc/groups/ahamah-public/@wcm/@sop/@smd/documents/downloadable/ucm_458896.pdf p8. Accessed December 2016.
The Conversation
The Case against Sugar Isn’t So Easily Dismissed
I believe a critical point has been lost in the responses to my lead essay. My concern in my essay and my books is a simple and regrettable fact: the epidemics worldwide of obesity and diabetes that occur whenever populations pass through a nutrition transition from a traditional diet and lifestyle, whatever that may be, to a western one. Something is causing that, and because obesity and diabetes, particularly type 2, are intimately linked to insulin resistance, we should be looking ultimately and desperately for the cause of insulin resistance. Geneticists would say we’re looking for the environmental trigger that reliably and often dramatically increases the prevalence of the obese and diabetic phenotype, regardless of the underlying human genotype. And because insulin resistance, obesity, and diabetes are all intimately linked to heart disease, that trigger is almost assuredly going to be a cause of coronary heart disease as well.
But in this country, nutrition and chronic disease research from the 1950s onward was obsessively focused on a very different question: the dietary cause of heart disease in the United States and Europe. When the researchers decided on the basis of exceedingly premature evidence that dietary fat was the culprit, that drove all public health debates and thinking ever after. Even hypotheses about the cause of obesity and diabetes had to be reconcilable with the belief that saturated fat caused heart disease. As such, the evidence implicating insulin resistance in the disorder (and so the carbohydrate content of the diet) was delayed by 30 years in its acceptance, as I discussed in Good Calories, Bad Calories. Its implications are still not accepted because they clash with what remains of the dogmatic belief that saturated fat causes heart disease. And this all happened because researchers were asking the wrong question (and they got the wrong answer even to that): “why CHD in America now,” rather than “why obesity, diabetes, and insulin resistance in populations worldwide whenever they westernize?”
Sugar and refined grains seemed to be the most likely answer to the right question, but this was swept under the rug or pronounced quackish because that answer also didn’t square with the saturated fat hypothesis. The key to all good science is understanding the question you’re asking and how it relates to the answers you need to find. And this problem is manifested once again in the responses of Drs. Guyenet and Freedhoff.
Now that we’re almost literally neck deep in obesity and diabetes, the right question is vitally important to answer. If the sugar hypothesis is wrong, it is critically important that it be refuted definitively. That can only happen on the strength of far, far stronger evidence than Dr. Guyenet provides in his somewhat flip and casual response. And if the sugar hypothesis is unambiguously refuted, whatever hypothesis steps up as the next prime suspect has to be very carefully considered. (i.e., not the simplistic notion that people eat too much and move too little). We need a hypothesis that holds the promise of explaining the epidemics everywhere.
In stopping an epidemic, nothing is more important than correctly identifying its cause. Where we are today with obesity and diabetes reminds me of where infectious disease specialists were through most of the 19th century, when they blamed malaria and other insect-born diseases on miasma, or the bad air that came out of swamps. That was mildly effective, in that it was an explanation for why the rich in any particular town preferred to build their homes on hills, high above the miasma and, incidentally, away from the swamps and lowlands and slums where the vectors of these diseases were breeding. But only by identifying the vectors and the actual disease agents do we help everyone avoid them and eradicate the diseases. Only by unambiguously identifying the cause can we effectively design treatments to cure it. The kinds of explanations that Dr. Guyenet and Freedhoff put forth – highly palatable foods or ultra-processed foods – are the nutritional equivalents of the miasma explanation. They sound good; they might help some people incidentally eat the correct diets or offer a description of why other people already do, but they’re not the proximate cause of these epidemics. And there is a proximate cause. We have to find it. I can guarantee it’s not saturated fat, regardless of the effect of that nutrient on heart disease risk. What is it?
Now I am going to focus primarily on Dr. Guyenet’s response, as his was by far the most antagonistic, questioning both the history I present in the lead essay as well as the conclusions I’ve derived from the history and the science. While Dr. Guyenet does indeed challenge “specific and testable assertions” related to my lead essay, the one assertion he does manage to refute successfully is not, regrettably, an assertion I made in the article. As for the rest, the evidence against is not nearly as compelling as he presents it.
First, Dr. Guyenet examined “the 1980 Dietary Guidelines to determine if they condemn fat and take a weak stance on sugar as suggested.” He then set out to determine whether the 1980 Guidelines contributed to obesity, diabetes, and coronary heart disease. He concluded that they didn’t.
I was under the impression when I wrote the essay, though, and still am upon re-reading it, that I do not make such a simplistic assertion. The point that I made is not about the 1980 USDA Guidelines alone – Dr. Guyenet and I both note that they urged readers to avoid too much sugar – but rather the entire movement of the research community to demonize fat, and the journalistic coverage of it, and the series of government documents, and the consensus conferences that followed along because of it—all part of the same concerted public health effort that led us by the late 1980s to believe that the essence of a healthy diet is its relative absence of fat and saturated fat. As an unintended consequence, this ill-conceived dogma-building directed attention away from the possibility that sugar has deleterious effects independent of its calories.
These government reports, as I noted, included the FDA GRAS report on sugar in 1986, the Surgeon General’s Report on Nutrition and Health in 1988, the National Academy of Sciences Diet and Health report in 1989, the British COMA report on food policy the same year, and others. I could have also mentioned the 1984 NIH consensus conference on “lowering blood cholesterol to prevent heart disease” that followed on this legendary Time Magazine cover – “Cholesterol, And Now the Bad News” – and the founding in 1986 of the National Cholesterol Education Program, which published its guidelines for cholesterol lowering the following year. All focused on dietary fat and serum cholesterol as the agents of heart disease and all mostly or completely ignored the evolving science on insulin resistance and metabolic syndrome that implicated sugar and other processed carbohydrates.
Indeed, if anything, the more relevant of the two USDA Dietary Guidelines, the one that Dr. Guyenet does not address, is the 1985 version that declared without a caveat, as I noted, that “too much sugar in your diet does not cause diabetes.” This is, of course, remains the critical question and the one that yet has to be rigorously tested (ignoring the tautology implied by the use of the words “too much”).
Dr. Guyenet, Dr. Freedhoff, and I all agree that had Americans eaten as the guidelines cautioned (and just as Michael Pollan would have preferred as well), we’d all very likely be healthier. But we didn’t. The question is whether the dietary fat/serum cholesterol/heart disease obsession directed attention away from the hypothesis that sugar causes heart disease, diabetes, and perhaps obesity as well through its effect on insulin resistance. The secondary question is whether this obsession in government documents, programs, journalistic coverage, and (pseudo)scientific reviews explains why we continued to eat such high sugar diets. As Dr. Guyenet notes, Americans still consume a significant amount of our calories from grain-based desserts and sugary beverages. But why? By focusing on the straw man of the 1980 guidelines, Dr. Guyenet fails to address that question. That he’s taking on a straw man makes me thinks he’s more interested in appearing to win an argument than in dealing with what may be the single most important public health issue of our era.
A key point to make, as Professor Kealey does, is that Americans did indeed respond to the dietary dogma of the 1970s and 1980s by changing their diets. Dr. Freedhoff and Dr. Guyenet are wrong in this regard when they attend only to the total percentage and amounts of fats, carbohydrates, and protein in our diets, and not the type of fats, carbohydrates, and even protein. Looking at what we ate instead of how much we ate supports the supposition that Americans heard the advice on fat and acted on it, even as we were ignoring the sugar advice. As the USDA reports, between 1970 and 2005, we cut down on our use of butter (-17%) and lard (-66%), while almost doubling vegetable oil consumption (from 38.5 pounds per capita yearly to 73.7); we more than doubled how much chicken we ate (33.8 pounds per capita yearly to 73.6, probably skinless white meat, but I’m speculating), while reducing our red meat consumption by 17 percent, and beef by 22 percent. We cut back on eggs, too. So while total fat consumption decreased only marginally, as Drs. Freedhoff and Guyenet note, that marginal decrease is accompanied by a reduction in animal fats and their replacement by vegetable oils, which were thought to be heart healthy and still are (perhaps also erroneously). The type of fats we consumed and the type of foods we consumed changed significantly, and this change was very much in accord with what we were being told.
The post-1980 focus on dietary fat also led to the creation and sale of thousands, perhaps tens of thousands, of non-fat and low-fat food-like substances (credit for the terminology once again to Mr. Pollan). In this instance, the CDC’s publication Healthy People 2000 is informative: Healthy People 2000 included multiple “nutrition objectives” aimed at reducing dietary fat consumption, including the creation of 5,000 low-fat or low-saturated fat products. It included nutrition objectives to reduce salt intake and increase complex carbohydrate and fiber consumption, but included no such objective for sugar or sugar-rich foods. Why not? Indeed, I find that the words “sugar” or “sugars” appear only five times in the almost 400-page final review of how well the guidelines were met. In 1995, the American Heart Association counseled in one of its pamphlets that Americans could control the amount and kind of fat consumed by “choos[ing] snacks from other food groups such as…..low-fat cookies, low-fat crackers,…unsalted pretzels, hard candy, gum drops, sugar, syrup, honey, jam, jelly, marmalade (as spreads).” In 2000, the AHA published this cookbook of low-fat and luscious sugar-rich “soul-satisfying” desserts. I don’t know if Dr. Guyenet would describe this as a “weak stand” on sugar or not, but it does shed light on our failure to limit sugar consumption during a period in which all public health advice was focused on reducing fat.
The more important question, and a very different one, is whether our sugar consumption has uniquely deleterious effects on our health. To refute the claim that consuming sugar might cause heart disease, Dr. Guyenet points out that heart disease mortality has dropped precipitously over the years of the obesity and diabetes epidemics and during a period when sugar consumption clearly increased (technically “caloric sweeteners” since the increase was due primarily to high-fructose corn syrup). Professor Kealey makes a similar point but with a far more nuanced perspective about how mortality rates are confounded by what are, after all, a half-century’s worth of very concerted efforts by medical researchers, the pharmaceutical and medical industry, and public health authorities to reduce mortality. That these efforts succeeded in reducing mortality is indeed commendable, but it makes it far more difficult than Dr. Guyenet suggests to derive meaning from the mortality data. If it’s evidence against the sugar hypothesis, it’s very weak evidence.
Dr. Guyenet references a 2007 article that applies a statistical model to assign proportions of the declining mortality to a variety of causal factors. Aside from the usual problem with models (all are wrong, some are useful, as the statistician George Box famously put it) the authors note that even in the model they employed, the declines in mortality that they observed “were partially offset by increases in the body-mass index and the prevalence of diabetes.” This would be expected if sugar consumption is a causal factor in obesity and diabetes, as proposed in my books. Hence I fail to see how this evidence would hold up in any court, science or law, as a reason to exonerate sugar.
Professor Kealey’s reference – a 2013 statement from the American Heart Association and American Stroke Association – is far more skeptical, and rightly so, about what can and cannot be concluded from the mortality data. It says, regarding the decrease in stroke mortality, all of which would be relevant to heart disease mortality as well:
These significant improvements in stroke outcomes are concurrent with cardiovascular risk factor control interventions. Although it is difficult to calculate specific attributable risk estimates, efforts in hypertension control initiated in the 1970s appear to have had the most substantial influence on the accelerated decline in stroke mortality. Although implemented later, diabetes mellitus and dyslipidemia control and smoking cessation programs, particularly in combination with treatment of hypertension, also appear to have contributed to the decline in stroke mortality. The potential effects of telemedicine and stroke systems of care appear to be strong but have not been in place long enough to indicate their influence on the decline. Other factors had probable effects, but additional studies are needed to determine their contributions.
Even Dr. Guyenet’s 2014 reference – “Challenges of Ascertaining National Trends in the Incidence of Coronary Heart Disease in the United States” – concludes with a statement that is difficult to reconcile with his confidence that this evidence tells us anything meaningful about the hypothesis that sugar is a cause of insulin resistance and so heart disease. The studies discussed, the authors write in the last two sentences, “yield encouraging but tentative signals that the incidence of CHD in the United States may be waning. Bringing greater clarity to this important topic of cardiovascular epidemiology poses a pressing public health need.”
In Dr. Guyenet’s commentary, he concludes with what he considers strong evidence to refute the hypothesis that sugar consumption is a unique cause of obesity and so, by association, diabetes. It is, he says, the results of an experiment in which an entire nation cuts its sugar consumption with the outcome of interest being the national prevalence of obesity. Here’s Dr. Guyenet’s evidence:
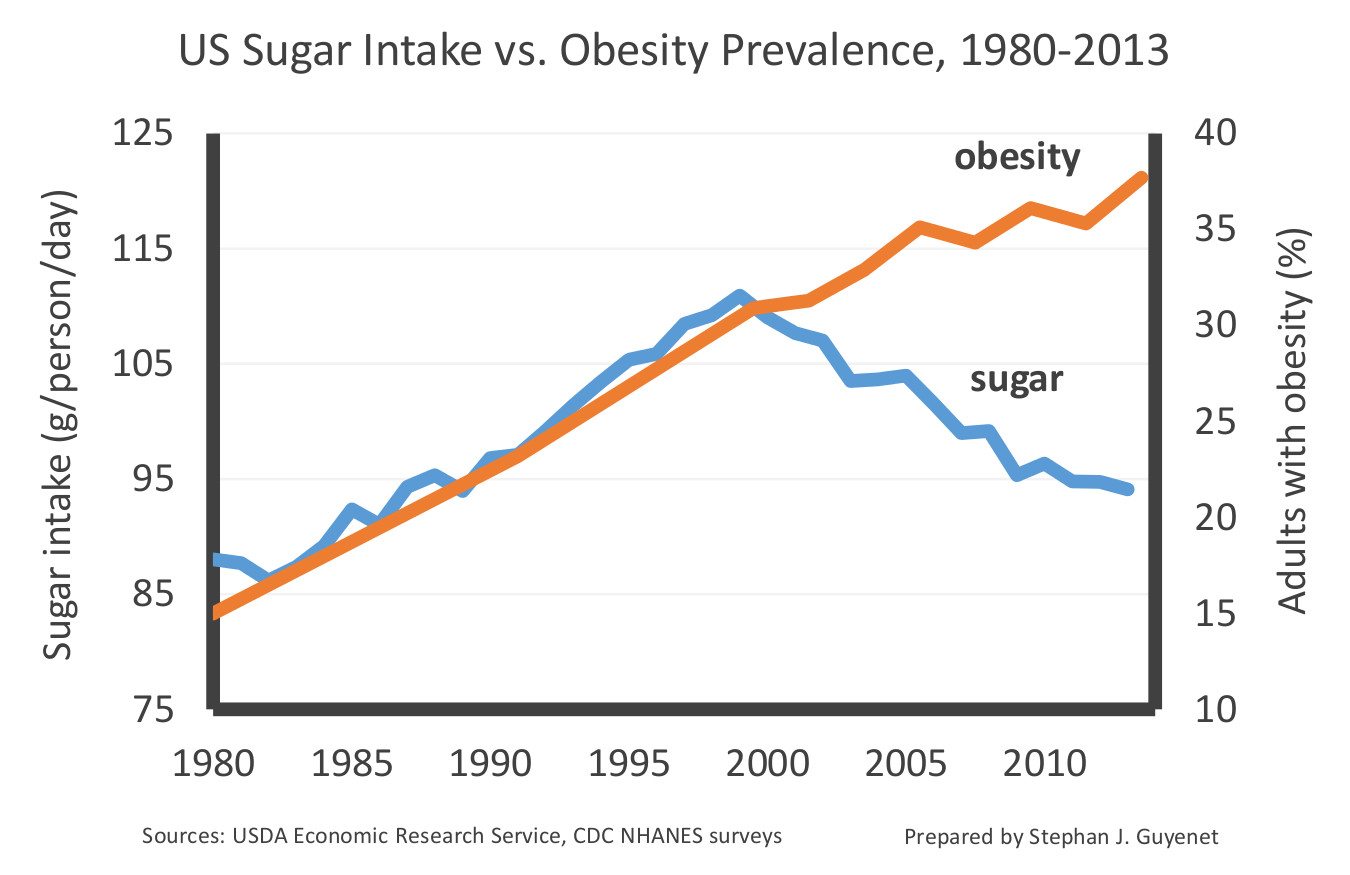
Considering the diverging trends in this chart post-1999, Dr. Guyenet writes, “Americans have been reining in our sugar intake for more than fourteen years, and not only has it failed to slim us down, it hasn’t even stopped us from gaining additional weight.”
A minor point is that Dr. Guyanet’s chart is deceptive. Dr. Guyenet inflates the sugar intake scale, such that a modest 15 percent decline in relative sugar intake is comparable in scale to what would be a dramatic forty percent decline in the relative prevalence of obesity. In doing so, he makes the reining in of sugar consumption since 1999 look more dramatic than it might otherwise look. Had he kept the scales more equitable, we could have imagined why a modest drop of 15 percent in sugar consumption might do little to stem the tide in obesity.
To help understand why not, let’s imagine a similar situation with cigarettes and lung cancer. Would we expect a 15 percent decline in cigarettes smoked per capita – say from 20 cigarettes a day to 17 – to lead to an immediate decline in lung cancer incidence or even to a stemming of the tide? And would Dr. Guyanet then conclude: “this suggests that cigarette smoking is highly unlikely to be the primary cause of lung cancer in the United States?” I’m going to go out on a limb here and say I kind of doubt it.
We can use a similar chart from the lung cancer/cigarette experience to further demonstrate the problem with Dr. Guyenet’s simplistic assumption that every cause has to be promptly and linearly associated with its effect. Here’s a chart, courtesy of the CDC, showing per capita cigarette consumption in the U.S. – which peaked in 1965, the year after the Surgeon General’s report on smoking and health – and per capita lung cancer rates, which took thirty years to turn over and head downward.
And here’s a part of that chart blown up, using Dr. Guyenet’s color scheme, to make what Dr. Guyenet would seemingly argue is a case against cigarettes as a primary cause of lung cancer.
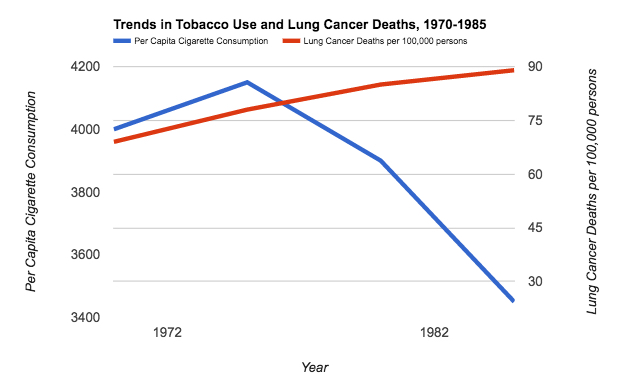
It would indeed be nice if our bodies, both on a population-wide and individual basis, responded immediately to the removal of a toxic substance from the environment. But there are many reasons why they wouldn’t, among them being threshold effects, intergenerational effects (the passing down of a predisposition to become obese and diabetic from mother to child in the womb, as documented in the Pima population and discussed in my books) and an incubation period for development of the disease, of the kind that explains the smoking and lung cancer delay. As I noted in my 2007 book, Good Calories, Bad Calories, after studying the diabetes epidemics among local ethnic groups in the 1950s, the South African diabetologist Dr. George Campbell suggested both a 20-year gestation period (similar to lung cancer), and increasing rates of diabetes in populations so long as consumption was above a 70 pounds per capita per year threshold.
Considering both the American Heart Association and the World Health Organization now suggest that a healthy diet should contain no more than about 50 pounds of sugar yearly, and ideally half that, and consider we’re still at a population level well above 70 pounds, it’s a safe bet that we wouldn’t expect a downturn in obesity quite yet from the data Dr. Guyenet provides.
It’s this kind of simplistic argument and a lack of understanding of the very obvious limitations of observational and epidemiological data that I have argued in my books got us into this dire public health situation. What we all need are more informed and nuanced and, yes, skeptical discussions of what the evidence can and cannot establish to get out of it.
Dr. Freedhoff takes a different tack, suggesting not that I’m simply wrong, as Dr. Guyenet does, but that I’m missing a point that is all too clear to a working physician. When he notes that there were flaws in the science of the case against dietary fat, and that such flaws are also present in the sugar data, he is echoing the points I make in my book on sugar. That I am nervous about government regulation of sugar and sugary products is at least partly for this reason.
Dr. Freedhoff is right that I believe that the only way to stop an epidemic is to first unambiguously identify the cause, and my book and this article are about the possibility that sugar is it. I do not believe “ultraprocessed” foods are responsible or even a meaningful way to identify what is the cause. Certainly not, if they’re defined as “ready to consume (or heat) formulations manufactured from cheap ingredients.” If we go looking for them, which is always a good idea, we can find epidemics of obesity and diabetes in the literature in populations going back more than a century, in which such ready to consume formulations did not exist. What these populations had, though, was sugar, white flour, and maybe alcohol, and these were new additions to their diets. It’s possible that because my training is in physics and Dr. Freedhoff’s is in medicine that we just assign a different value to the usefulness of Occam’s razor in establishing reliable knowledge. I believe these historical populations, enumerated in my second book, Why We Get Fat, can be used to rule out suspected causes including ultraprocessed food, however that’s defined. Dr. Freedhoff finds them less valuable, and we have discussed this in the past.
Dr. Freedhoff is concerned with the advice he should give his patients to maximize their health, which includes maximizing their happiness. I’m concerned with identifying the causes of the epidemics such that we know what has to be done to stop them. If sugar is the ultimate cause of obesity and diabetes, however, which is at least a viable hypothesis, then I can’t agree with Dr. Freedhoff that his advice to his obese and diabetic patients should not include making this fact abundantly clear.
This is why I often evoke cigarettes as a comparison. Because, based on solid evidence, we are confident that smoking causes lung cancer, we do not advise smokers to smoke in moderation or to worry that non-smoking will make them unhappy. (It certainly will, at least in the short run. I can personally vouch for that.) We don’t assume that if we tell them that cigarettes cause lung cancer, this will reduce the likelihood that they’ll quit, because changing their behavior for their own good may be an unrealistic luxury for them. We give them the knowledge and we let them decide. We don’t say, “what’s the smallest amount needed to be happy?” as Dr. Freedhoff suggests about dietary indulgences. We counsel, as Dr. Freedhoff also does, “not smoking.”
While Dr. Freedhoff’s seven behaviors may make for a happier life, they may direct the attention of his patients away from precisely those behaviors (i.e., eating of certain foods) that triggered their condition. Moreover, his claim that the behaviors he does advise will bestow “incredible health benefits” is as bereft of science as his worries about targeting sugar. I doubt we need clinical trials to suggest we’ll be healthier and happier if we get a good night’s sleep and nurture our relationships, but to assume that obese and diabetic people don’t, and to make this the basis of treatment for people who come to Dr. Freedhoff to be helped, seems condescending. We have our mothers and our friends to give us that advice. What we need our doctors to tell us (correctly) is why we got fat, and why we got diabetes, and what we can do to reverse it. And then it will be up to us to decide if we want to follow that advice.
Finally, I would like to thank Professor Kealey for the kind words and his thoughtful assessment. I would take issue with one statement, which is whether or not I am the most influential journalist in the nutrition area. I would have voted for Michael Pollan in that regard, although it is possible that he might vote for me. In doing so, as he did in a recent article, he might leave it ambiguous whether my contribution is ultimately to the benefit of our health, or the harm.
Extraordinary Claims Require Extraordinary Evidence
Taubes makes a number of arguments in his response to my piece that merit dissection, but for the sake of being concise I will respond only to those that are the most important. Let’s focus on the primary bone of contention first, which is Taubes’s extraordinary claim about sugar. The claim in question is that sugar is the primary cause of obesity and common noncommunicable diseases such as cardiovascular disease and diabetes, and that other causes such as calorie intake, physical activity, and other aspects of diet quality are not important.
Taubes states that “If the sugar hypothesis is wrong, it is critically important that it be refuted definitively.” It is not the responsibility of the scientific community to refute every hypothesis that emerges from the popular press; if Taubes believes his extraordinary claim is correct, the onus is on him to provide extraordinary evidence in support of it. What is his evidence?
Taubes’s first piece of “evidence” is the assumption that obesity and most noncommunicable diseases are caused by one factor. This is based on a tool of logic called Occam’s Razor. Allow me to explain how Occam’s Razor works: All else being equal, the simpler of two hypotheses is most likely to be correct. The key phrase here is “all else being equal.” Occam’s Razor is a tie breaker at best, not a trump card that can be used to discard experimental evidence that challenges one’s hypothesis.
Having established that Occam’s Razor cannot be used to discard evidence, let’s consider what this evidence currently suggests about sugar:
- Sugar can increase body fatness, and this depends entirely on its ability to increase calorie intake.(1)
- A high intake of sugar does not impede weight loss when calorie intake is reduced.(2)
- Realistic doses of sugar have a modest negative impact on markers of diabetes risk, and this is potentiated by excess calorie intake.(3)
- Realistic doses of sugar have a modest negative impact on markers of cardiovascular disease risk.(4)
- Sugar is not very fattening in animal models of obesity, and its effects on body fatness and insulin resistance are generally less than those of added fat alone; the combination of sugar and fat is more harmful than either in isolation.(5–7)
- Various forms of sugar intake are often associated with weight gain in observational studies, among other factors, but the associations are inconsistent and generally not strong.(1)
- Refined sugar and/or sugar-sweetened beverage intake is associated with coronary heart disease risk, among many other factors such as low physical activity level, low fruit and vegetable intake, low nut intake, low dairy intake, and dietary fat quality.(8–11)
In aggregate, this evidence does not lend itself to the hypothesis that sugar is the primary driver of obesity or noncommunicable disease risk, although it does support the conventional hypothesis that refined sugar plays a role in obesity and noncommunicable disease, among other factors.
Taubes states that “because obesity and diabetes, particularly type 2, are intimately linked to insulin resistance, we should be looking ultimately and desperately for the cause of insulin resistance.” While Taubes continues his quest to uncover the causes of insulin resistance and type 2 diabetes, the scientific community has already identified them: Excess body fatness, physical inactivity, and genetics (12–19). This fact is supported by multiple long-term human trials demonstrating that even modest weight loss via calorie restriction and exercise reduces the incidence of type 2 diabetes by more than half (12–17). No such evidence exists for sugar.
Here is more evidence demonstrating that the factors Taubes believes to be unimportant are in fact central to insulin resistance and type 2 diabetes:
- Increasing calorie intake increases body weight, and this produces marked insulin resistance (20,21).
- Conversely, decreasing calorie intake decreases body weight and this substantially decreases insulin resistance (22).
- A long-term primate study suggests that calorie restriction markedly reduces the risk of diabetes and cardiovascular disease over the course of the lifespan (23). Human studies suggest that the same is likely true for us (24).
- Physical inactivity rapidly produces marked insulin resistance, and physical activity rapidly reverses it (25,26).
Rather than providing extraordinary evidence to support his extraordinary claims about sugar, Taubes offers weak evidence while omitting strong evidence to the contrary. So where, exactly, do his bold opinions on sugar come from? As it turns out, they come in large part from the very form of evidence he decries in his latest piece.
In response to my graph demonstrating that obesity has increased in the United States even as sugar intake has decreased, Taubes states “It’s this kind of simplistic argument and a lack of understanding of the very obvious limitations of observational and epidemiological data that I have argued in my books got us into this dire public health situation.” This statement is rather interesting since observational evidence is at the foundation of his own argument about sugar, and he cites observational evidence repeatedly in his books and in the very piece from which I drew that quote.[1]
A key argument of Taubes’s latest book, The Case Against Sugar, as well as his previous two books and his current response, is that observational evidence from cultures around the globe can tell us which factors are responsible for obesity and noncommunicable disease, and which factors aren’t. Here is how Taubes describes the argument in his current response: “I believe these historical populations, enumerated in my second book, Why We Get Fat, can be used to rule out suspected causes including ultraprocessed food, however that’s defined.”
This type of population-level observational evidence is called “ecological evidence.” Apparently Taubes considers it sufficiently robust to rest his own beliefs upon, yet when others cite similar evidence they are failing to appreciate its “very obvious limitations,” and they may even be precipitating a public health crisis.
If ecological evidence is admissible, as Taubes’s writing suggests it is, then perhaps we should see if there are any cultures that refute his assertion that obesity and chronic disease pop up anytime a high intake of sugar does. These are not difficult to find: The Hadza, a well-studied hunter-gatherer tribe in Tanzania, has a year-round average sugar intake from honey and fruit that approximates that of Americans (27). Yet they show no sign of obesity, diabetes, cardiovascular disease, or any of the other conditions Taubes attributes to sugar (28).
It is rather unclear to me, and to others who are familiar with the scientific literature on insulin resistance, obesity, chronic disease, and nutrition, how Taubes arrived at such an extreme position. The best I can gather from his most recent book and his writing here is that his belief originates primarily from Occam’s Razor and observational evidence. If Taubes has extraordinary evidence supporting his extraordinary claim about sugar, then perhaps this would be a good time to share it.
The Infamous Graph
In my initial response to Taubes, I presented evidence that sugar intake has been declining since 1999, while obesity and diabetes rates have continued to increase (this decrease in sugar intake is supported by multiple independent lines of evidence) (29–33). Taubes focused on the axes of the graph I presented, suggesting that the scale is misleading because it exaggerates the magnitude of the change in sugar intake. Allow me to restate what I explained in the graph’s legend: the purpose of the choice of scale was not to illustrate the magnitude of the changes in question, but rather to illustrate the correlation between obesity and sugar intake over time. Thus, I selected a scale that would allow a general audience to easily see the correlation of the two factors pre-1999, and the divergence post-1999. See below:
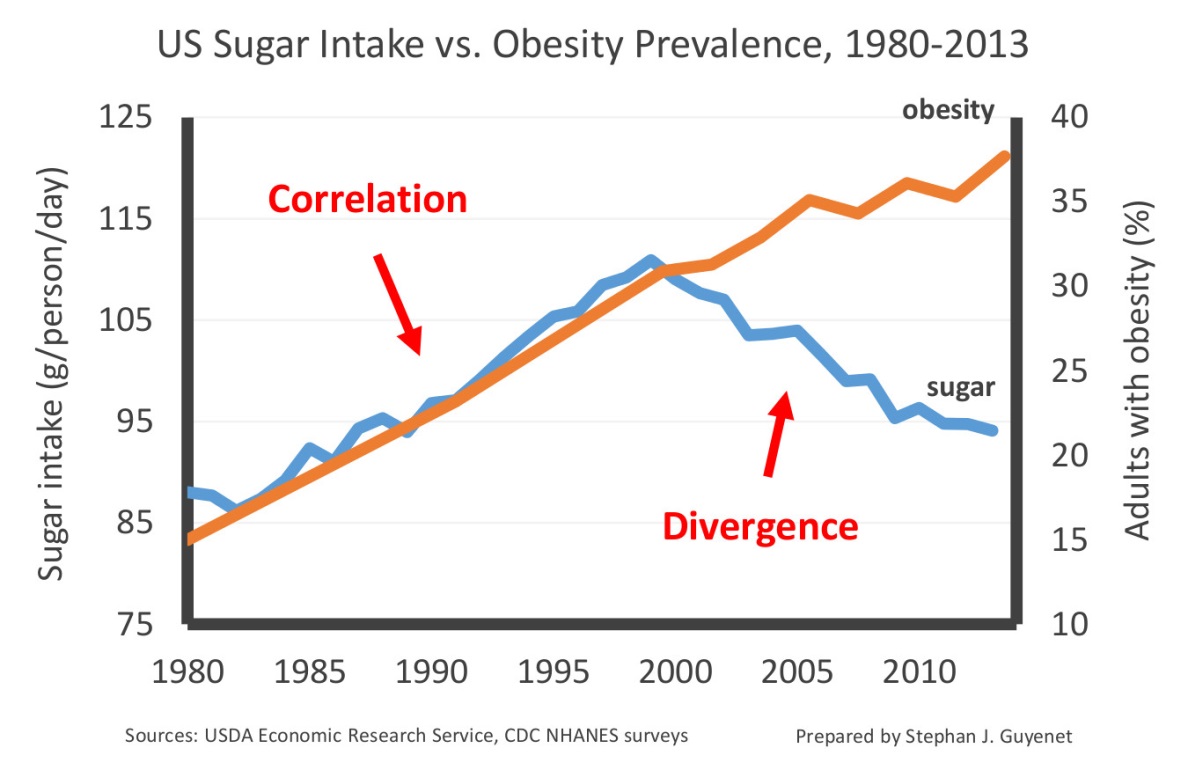
Taubes’s suggestion that I was attempting to exaggerate the decline in sugar intake is also difficult to understand because I stated its magnitude in the text: 18 percent. For reasons that are unclear, he shrinks this number to “a modest drop of 15 percent” in his response. Other sources indicate that sugar intake may actually have declined by up to 23 percent, and that sugar intake is either stable or decreasing in most countries globally even as obesity and diabetes rates continue to climb (34).
In any case, focusing on how I chose to construct my graph is a diversion from the real crux of the argument: The observation that sugar intake has been declining since 1999 and obesity and diabetes rates have not only failed to decrease, but continued to climb, is difficult to reconcile with the hypothesis that sugar is the primary cause of these conditions. Yet Taubes nimbly evades falsification by suggesting that the sugar we ate decades ago may be continuing to fatten us today. Does it matter that there is precisely no evidence to support this claim?[2] I happen to think so.
The Decline of Heart Attack Risk: Fact or Fiction?
Taubes does not attempt to defend his initial assertion that sugar is the primary cause of coronary heart disease. Instead, he argues that my piece attempted to “refute the claim that consuming sugar might cause heart disease,” and he disputes the evidence cited. Allow me to point out that I clearly stated in my piece that refined sugar likely contributes to coronary heart disease, and that the evidence I cited “doesn’t exonerate sugar.”
The issue at hand is not the uncontroversial proposition that refined sugar contributes to coronary heart disease. It is Taubes’s extraordinary claim that sugar is the primary cause of this disease, a claim for which he has provided no credible evidence.
Taubes does not feel sufficiently compelled by the evidence I presented demonstrating that coronary heart disease mortality has declined by more than 60 percent over the same period of time that sugar intake has increased. He notes correctly that mortality data can be confounded by advances in medicine. As I explained in my initial piece, advances in medicine are insufficient to account for this change, but even so, let’s consider a harder form of evidence: Autopsy data. This directly measures the presence of atherosclerosis in the coronary arteries, which is the definition of coronary heart disease.
At least two independent autopsy studies have been conducted over the time period in question, and both reported the same principal finding: Coronary artery disease decreased during the 1980s and 1990s as sugar intake was increasing (35,36). It is particularly telling that this decrease was also observed among younger people who were unlikely to be receiving medical therapy for heart disease.
This decline in coronary heart disease is not hard to explain. It is consistent with the decline of cigarette smoking and favorable changes in blood lipids, two well-established risk factors. (37) As Taubes notes, increases of obesity and diabetes may reverse this trend due to their impact on cardiovascular risk factors. Yet there is no evidence that sugar is the primary driver of this.
The Changing American Diet
In his response, Taubes cites observational data on U.S. food intake to support his contention that government dietary advice influenced American eating habits. Given his distaste for the “very obvious limitations” of observational evidence, it is unclear why he assumes that this association implies a causal effect of dietary advice on American eating habits.
It is true that the American diet has changed substantially over the course of the last 50 years, but these changes are not as easy to attribute to “dietary dogma” as Taubes assumes. In fact, the food and agriculture industries underwent substantial changes over the period in question that likely contributed to these shifts. For example, the inflation-adjusted cost of poultry plummeted, as did the cost of refined seed oils such as soybean oil. At the same time, the rise of industrially processed foods increased demand for cheap, stable, liquid fats such as soybean oils. Hydrogenated fats provided a cheaper and more stable alternative to lard and butter. In this context, it is not surprising that chicken and seed oils became more prevalent, at the expense of more costly and less convenient foods like butter, lard, and beef. It is certainly possible that cautions about saturated fat and cholesterol contributed to these changes, but this is not so clear since absolute saturated fat and cholesterol intake did not actually decline over the period in question.(29)
In any case, these details are a distraction from the main thrust of Taubes’s argument: dietary fat was “demonized” and sugar was “ignored,” and this explains why we eat so much sugar. As explained in my previous piece, dietary fat intake has not declined at all (not even “marginally” as Taubes states), and government dietary advice consistently recommended limiting sugar intake. These facts are difficult to reconcile with Taubes’s narrative.
Taubes implies that misguided advice from researchers and public health officials explains the fact that grain-based desserts like cake are the number one source of calories in the United States. As I explained in my last piece, we don’t eat cake and pizza because we’ve been snookered by researchers into thinking they will trim our waistlines. We eat them because we like them, despite the known consequences. Taubes continues to blame our junk food habit on the research and public health communities when common sense suggests otherwise.
Wrath of the Guidelines Redux
Taubes states that in his initial essay, he was not simply arguing that the USDA Dietary Guidelines caused us to eat more sugar or contributed to the epidemics of obesity and diabetes, but that the Guidelines were part of a broader “movement by the research community to demonize fat.” I accept the premise that his argument was not focused exclusively on the Guidelines, however the Guidelines clearly played an important part in it, as demonstrated by the first paragraph of his essay and a sentence from the second paragraph:
Forty years ago this month, January 1977, the federal government entered the business of giving dietary advice, first with a Congressional report released by George McGovern’s bipartisan Select Committee on Hunger and Human Needs, which in turn prompted the first Dietary Guidelines from the U.S. Department of Agriculture… While McGovern, his colleagues, and their committee staff may have all hoped the guidelines would lead to a nation eating, perhaps, as Michael Pollan would later memorably put it, (whole) food, “mostly plants and not too much,” that would not be the case.
Taubes asserts that the scientific and public health communities “demonized” fat and “ignored” sugar, a black and white narrative that does not fit the facts. As I demonstrated in my previous response, this bold assertion is not consistent with the equal attention paid to fat and sugar in the 1980 Guidelines—the document that was the primary interface between government dietary policy and the public. The Guidelines recommended that Americans “avoid too much” of both, a statement that does not demonize or ignore either one.
In any case, although history is not as black and white as Taubes suggests, I agree that the general cultural climate was to overemphasize dietary fat in the 1960s through the 1990s, at the expense of other important factors. The scientific and public health communities learned the hard way not to place undue emphasis on one nutritional factor, particularly in the absence of definitive evidence. I hope Taubes will not drive the U.S. public to repeat this mistake of history.
[1] For example, the observation that government diet recommendations coincided with changes in the U.S. diet. This association is assumed to be evidence of a cause-and-effect relationship between the two.
[2] Taubes cites evidence that certain health effects (e.g., lung cancer) can be separated from the exposure (e.g., cigarette smoke) by decades. But establishing that a delayed effect is biologically possible is not the same thing as establishing that it actually occurs for the particular exposure in question. Taubes cites evidence of intergenerational effects of obesity and metabolic disease, but these experiments are not relevant to the effects of sugar specifically.
Sources
1. Te Morenga L, Mallard S, Mann J. “Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies.” BMJ. 2012 Jan 15;346:e7492.
2. Surwit RS, Feinglos MN, McCaskill CC, Clay SL, Babyak MA, Brownlow BS, et al. “Metabolic and behavioral effects of a high-sucrose diet during weight loss.” Am J Clin Nutr. 1997 Apr;65(4):908–15.
3. Horst KW ter, Schene MR, Holman R, Romijn JA, Serlie MJ. “Effect of fructose consumption on insulin sensitivity in nondiabetic subjects: a systematic review and meta-analysis of diet-intervention trials.” Am J Clin Nutr. 2016 Dec 1;104(6):1562–76.
4. Te Morenga LA, Howatson AJ, Jones RM, Mann J. “Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids.” Am J Clin Nutr. 2014 Jul;100(1):65–79.
5. Surwit RS, Feinglos MN, Rodin J, Sutherland A, Petro AE, Opara EC, et al. “Differential effects of fat and sucrose on the development of obesity and diabetes in C57BL/6J and A/J mice.” Metabolism. 1995 May;44(5):645–51.
6. Sumiyoshi M, Sakanaka M, Kimura Y. “Chronic intake of high-fat and high-sucrose diets differentially affects glucose intolerance in mice.” J Nutr. 2006 Mar;136(3):582–7.
7. Lozano I, Van der Werf R, Bietiger W, Seyfritz E, Peronet C, Pinget M, et al. “High-fructose and high-fat diet-induced disorders in rats: impact on diabetes risk, hepatic and vascular complications.” Nutr Metab. 2016;13:15.
8. Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. “Sweetened beverage consumption and risk of coronary heart disease in women.” Am J Clin Nutr. 2009 Apr;89(4):1037–42.
9. de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. “Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men.” Circulation. 2012 Apr 10;125(14):1735–41, S1.
10. Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. “Added sugar intake and cardiovascular diseases mortality among US adults.” JAMA Intern Med. 2014 Apr;174(4):516–24.
11. Willett MDWC, Skerrett PJ. Eat, Drink, and Be Healthy: The Harvard Medical School Guide to Healthy Eating. 1 edition. New York: Free Press; 2005.
12. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. “Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.” N Engl J Med. 2002 Feb 7;346(6):393–403.
13. Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. “Effect of weight loss with lifestyle intervention on risk of diabetes.” Diabetes Care. 2006 Sep;29(9):2102–7.
14. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. “Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance.” N Engl J Med. 2001 May 3;344(18):1343–50.
15. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. “The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1).” Diabetologia. 2006 Feb;49(2):289–97.
16. Kosaka K, Noda M, Kuzuya T. “Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males.” Diabetes Res Clin Pract. 2005 Feb;67(2):152–62.
17. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. “Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study.” Diabetes Care. 1997 Apr;20(4):537–44.
18. Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. “Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men.” Diabetes Care. 1994 Sep;17(9):961–9.
19. Poulsen P, Kyvik KO, Vaag A, Beck-Nielsen H. “Heritability of type II (non-insulin-dependent) diabetes mellitus and abnormal glucose tolerance—a population-based twin study.” Diabetologia. 1999 Feb;42(2):139–45.
20. Erdmann J, Kallabis B, Oppel U, Sypchenko O, Wagenpfeil S, Schusdziarra V. “Development of hyperinsulinemia and insulin resistance during the early stage of weight gain.” Am J Physiol Endocrinol Metab. 2008 Mar;294(3):E568-575.
21. Sims E a. H, Horton ES. “Endocrine and Metabolic Adaptation to Obesity and Starvation.” Am J Clin Nutr. 1968 Dec 1;21(12):1455–70.
22. Larson-Meyer DE, Heilbronn LK, Redman LM, Newcomer BR, Frisard MI, Anton S, et al. “Effect of calorie restriction with or without exercise on insulin sensitivity, beta-cell function, fat cell size, and ectopic lipid in overweight subjects.” Diabetes Care. 2006 Jun;29(6):1337–44.
23. Colman RJ, Anderson RM, Johnson SC, Kastman EK, Kosmatka KJ, Beasley TM, et al. “Caloric restriction delays disease onset and mortality in rhesus monkeys.” Science. 2009 Jul 10;325(5937):201–4.
24. Fontana L, Meyer TE, Klein S, Holloszy JO. “Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans.” Proc Natl Acad Sci U S A. 2004 Apr 27;101(17):6659–63.
25. Hamburg NM, McMackin CJ, Huang AL, Shenouda SM, Widlansky ME, Schulz E, et al. “Physical inactivity rapidly induces insulin resistance and microvascular dysfunction in healthy volunteers.” Arterioscler Thromb Vasc Biol. 2007 Dec;27(12):2650–6.
26. Zierath JR. “Invited review: Exercise training-induced changes in insulin signaling in skeletal muscle.” J Appl Physiol Bethesda Md 1985. 2002 Aug;93(2):773–81.
27. Marlowe FW, Berbesque JC, Wood B, Crittenden A, Porter C, Mabulla A. “Honey, Hadza, hunter-gatherers, and human evolution.” J Hum Evol. 2014 Jun;71:119–28.
28. Raichlen DA, Pontzer H, Harris JA, Mabulla AZP, Marlowe FW, Josh Snodgrass J, et al. “Physical activity patterns and biomarkers of cardiovascular disease risk in hunter-gatherers.” Am J Hum Biol Off J Hum Biol Counc. 2016 Oct 9.
29. USDA Economic Research Service - Food Availability (Per Capita) Data System [Internet]. 2016 [cited 2016 Dec 22]. Available from: https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/
30. Fryar CD, Carroll MD, Ogden CL. “Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults Aged 20 and Over: United States, 1960–1962 Through 2013–2014.” Natl Cent Health Stat Health E-Stats. 2016 Jul.
31. Menke A, Casagrande S, Geiss L, Cowie CC. “Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012.” JAMA. 2015 Sep 8;314(10):1021–9.
32. Kit BK, Fakhouri THI, Park S, Nielsen SJ, Ogden CL. “Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010.” Am J Clin Nutr. 2013 Jul;98(1):180–8.
33. Makarem N, Scott M, Quatromoni P, Jacques P, Parekh N. “Trends in dietary carbohydrate consumption from 1991 to 2008 in the Framingham Heart Study Offspring Cohort.” Br J Nutr. 2014 Jun;111(11):2010–23.
34. Wittekind A, Walton J. “Worldwide trends in dietary sugars intake.” Nutr Res Rev. 2014 Dec;27(2):330–45.
35. Roger VL, Weston SA, Killian JM, Pfeifer EA, Belau PG, Kottke TE, et al. “Time trends in the prevalence of atherosclerosis: a population-based autopsy study.” Am J Med. 2001 Mar;110(4):267–73.
36. Nemetz PN, Roger VL, Ransom JE, Bailey KR, Edwards WD, Leibson CL. “Recent trends in the prevalence of coronary disease: a population-based autopsy study of nonnatural deaths.” Arch Intern Med. 2008 Feb 11;168(3):264–70.
37. Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. “Explaining the decrease in U.S. deaths from coronary disease, 1980-2000.” N Engl J Med. 2007 Jun 7;356(23):2388–98.
Complex Multi-Factorial Problems Tend Not To Have Simple Singular Causes
Perhaps it is my medical training that has me scratching my head in regard to Taubes’ argument that the only way to stop an epidemic is to unambiguously identify its cause. Not knowing the cause certainly didn’t stop Dr. John Snow back in 1854 when he determined that the source of the epidemic of fatal diarrhea plaguing London was a public water pump - the well of which had been dug just 3 feet from a cesspool. Though the bacterium Vibrio cholera had yet to be discovered, shutting down the pump stopped its fatal spread. Similarly I’m glad that Taubes wasn’t around then to discourage British sailors from bringing limes on their sea voyages because scurvy’s root cause had yet to be identified.
My head also needs some scratching when considering Taubes’ assertion that ultra processed foods aren’t drivers of chronic disease because there are examples of populations who had sugar and white flour in their diets but didn’t suffer diabetes or obesity. Putting aside the fact that sugar and white flour by themselves don’t meet the definition of ultra-processed foods (they instead fall into the category of “processed culinary ingredients”), pointing one’s finger at specific traditional populations’ diets to make a point is akin to trolling PubMed to find a study that agrees with you. I’m certainly not about to point to Hadzas’ diets, with 68% of their total calories coming from carbohydrates and 22% of those coming from honey, as being a useful means to prove that diets high in carbohydrates and honey are protective, the Hadzas’ lack of diabetes or obesity notwithstanding.
Perhaps it is also my medical training that has me recognize that unlike Taubes’ strawman suggestion that my advice is meant to “maximize” my patients’ happiness, my patients’ happiness does in fact matter, especially in regard to their diets, as food is not simply fuel. Food as pleasure is part of the human condition. We use food for comfort, for celebration, and no doubt as the world’s oldest social networking tool. It’s for these reasons, and the fact that we can’t simply stop eating, that Taubes’ smoking analogy falls short.
And what of Taubes’ assertion, despite his not likely ever having worked with people on behavior change, that the way doctors help patients is to, “give them the knowledge and let them decide”? While Taubes’ apparent vision of a physician is as a finger-waggling patriarch that provides black and white absolutist advice, real clinicians take the time to understand their patients and their lives. Real clinicians also appreciate the benefits of harm reduction. We understand that healthy living is challenged both by our modern toxic food environment as well as by a patient’s personal, socio-economic, and medical realities. We tailor our advice to each patient accordingly. And no, doing so is not seen as condescending.
Coincidentally, just after reading Taubes response I had the pleasure of seeing a patient who has taken to heart the advice to live the healthiest life that he can enjoy. Now no doubt he’s received a great deal of other advice from my office, but we’ve never asked him to cut out sugar, and he’s not on a low-carb diet (though some of our patients are - the ones who enjoy low-carb diets enough to sustain them). I asked him if I could share a bit of his story and he agreed. When we met in August he weighed over 300lbs and had just been discharged from the hospital following his admission for out of control type 2 diabetes. He was on 70 units of long acting insulin, along with a number of oral hypoglycemic drugs. His sugars were a mess; even with those 70 units of insulin and multiple oral hypoglycemic drugs, they were regularly clocking in at over 4 times normal. Six months later, he has lost over 40lbs, increased his exercise, improved his diet, is totally off insulin, and has sugars that are in the normal range. Most importantly, he doesn’t feel deprived. He is enjoying his life, and consequently he is confident that he’ll be able to sustain the behaviors he’s adopted. And his story is not even remotely unique. Sub-total weight loss, coupled with improved attention and guidance on big ticket healthy living behaviors, regularly leads to dramatic clinical benefits.
Which brings us, finally, to Occam’s Razor. Occam’s Razor dictates that the most plausible cause is likely the right one, but it’s important to point out that the most plausible cause is not necessarily the simplest. And here the most plausible cause for our rising rates of obesity and chronic non-communicable diet related diseases, as I elaborated in my first essay, is that we are eating much more than we ever have, that what we’re eating has changed dramatically, and that the world now more than ever markets and pushes nutritional chaff at every turn. These are causes that Taubes’ rebuttal did not address, and causes that would matter to anyone who understands that it’s not just the quality of calories that matter, but also their quantity.
While there’s no argument that sugar plays a real role in all of the above, and also no argument that it’s in public health’s best interest to work towards encouraging and enabling a societal reduction in the excessive consumption of sugar, dumbing everything down to one nutrient in an attempt to provide a simple solution to a highly complex and multi-factorial problem does a disservice to thoughtful public health strategies and to individual patient care.
Black and white is much more useful to dogma than doctors.
